Here is the rewritten section, crafted to sound completely human-written and natural, following the provided style guide and requirements.
Preventing a hospital readmission isn’t just about ticking boxes on a discharge checklist. It's about what happens after the patient goes home. It takes a real, coordinated effort to bridge that fragile gap between the controlled environment of a hospital and the unpredictable reality of a patient's own home. Get it right, and you prevent a world of pain and cost. Get it wrong, and the patient is right back where they started.
Why Hospital Readmissions Are a Critical Issue
Let's be clear: a hospital readmission is so much more than a number on a performance dashboard. For a patient, it’s a crushing setback. It’s the return of fear, pain, and the frustrating feeling that their recovery has failed. It often signals a breakdown somewhere in the care continuum, leaving them feeling completely overwhelmed and let down.
For the healthcare system, every single readmission is a sign of an opportunity missed. It’s not just a massive financial drain; it’s a failure to deliver care that sticks. The scale of this problem is staggering, with avoidable readmissions costing the U.S. healthcare system billions each year. Beyond the money, these returns put an immense strain on already overworked staff and tie up beds that are desperately needed for new emergencies. If we want to fix this, we have to start by understanding why these patients keep coming back.
The Human and Financial Cost of a Revolving Door
The ripple effect of a readmission is huge. Think about a patient just discharged after a heart failure event. They walk out with a handful of new, confusing prescriptions. If they can't afford a co-pay or misunderstand the new dosage schedule, their condition can spiral downward fast. Before you know it, they’re back in the ER. This cycle doesn't just damage their physical health; it chips away at their confidence to manage their own well-being.
A readmission often feels like a personal failure to the patient, but it’s almost always a system failure. It shines a harsh light on the gaps in communication, education, and support that happen during that delicate handoff from hospital to home.
This scenario plays out every single day. Most readmissions aren't caused by one big, dramatic event. They’re the result of small, preventable issues piling up.
Common culprits include:
- Medication Mix-Ups: Patients often get home and have no idea how to reconcile their old medications with the new ones. It’s a recipe for dosage errors.
- No Follow-Up in Sight: If a patient doesn't have a follow-up appointment scheduled with their primary doctor within a week of discharge, minor problems can quickly escalate.
- A Lack of Support: Many people, especially older adults, simply don't have a support system at home to help with meals, rides, or daily tasks. They're left to fend for themselves when they are at their most vulnerable.
- Ignoring the Red Flags: Patients often don't know the difference between a normal recovery symptom and a serious warning sign that requires a call to their doctor.
Each of these points is a place where we can—and must—intervene. When you look at the problem through the eyes of the patient and see the system-wide costs, the need for solid strategies to prevent hospital readmissions becomes undeniable. This isn't just about hitting a metric. It's about honoring our promise to see patients through to a full recovery.
Your Blueprint For A Strong Discharge Plan

Sending a patient home with a weak discharge plan is like sending them into a storm without a raincoat. That handoff is the single most critical moment in their care journey, and getting it right is your best defense against seeing them again for an unplanned return.
A truly solid plan doesn't get thrown together minutes before a patient walks out the door. It starts the moment they’re admitted. Kicking things off this early gives your team the runway needed to build a comprehensive, patient-centered strategy. It’s all about shifting from a reactive checklist to a proactive blueprint for a safe transition home. This means spotting potential barriers—like no transportation or confusion about new pills—long before discharge day ever arrives.
Start With Meticulous Medication Reconciliation
If there's one thing that drives readmissions, it's medication confusion. Patients often leave with a brand-new list of prescriptions, totally unsure how they mesh with what they were already taking at home. This is a recipe for errors, adverse events, and just plain not taking the meds.
Medication reconciliation is your fix. It's the disciplined process of creating one single, accurate list of every medication a patient is taking. You compare their home meds with the new ones prescribed during their stay and iron out any conflicts. This isn't just a job for the pharmacist; it's a team sport involving doctors, nurses, and the patient themselves. A clear, reconciled list is absolutely non-negotiable for preventing hospital readmissions.
A patient who truly gets their medications—what each one is for, how to take it, and potential side effects—is infinitely more likely to stick to the plan and sidestep complications.
This process is so crucial that it’s become a cornerstone of national quality initiatives. The federal government even put its weight behind it with measures like the Hospital Readmissions Reduction Program (HRRP), which financially incentivizes hospitals to nail down their care coordination with things like med reconciliation and solid patient education.
Secure The First Follow-Up Appointment
Never, ever let a patient leave without their first follow-up appointment already on the books. This one action creates a vital safety net, ensuring a seamless handoff from your care to their primary provider or specialist. Scheduling this for them lifts a huge weight off the shoulders of patients and their families.
Think about it. For someone feeling weak, overwhelmed, or just foggy from their hospital stay, the simple task of calling a doctor’s office can feel like climbing a mountain. When you handle it, you guarantee they get seen within that critical window—usually 7-14 days post-discharge—where problems can be caught before they spiral. This proactive step directly leads to better home health wound care patient outcomes and a smoother overall recovery.
Master The Teach-Back Method
Handing a patient a stack of papers and asking, "Any questions?" isn't education. It's a box-ticking exercise. To actually confirm they understand, you need to use the teach-back method. It’s a simple but incredibly powerful tool that shifts the focus from asking if they understand to asking them to explain it back in their own words.
For instance, you might try saying:
- "We’ve gone over a lot today. Just to make sure I did a good job explaining, could you tell me what symptoms would mean you need to call my office?"
- "So I can be sure we're on the same page, can you show me how you'll take these two new pills tomorrow morning?"
This isn’t a test of the patient's memory; it’s a test of how well you explained things. It turns a one-way information dump into a real conversation, building the patient's confidence and letting you catch misunderstandings before they can cause real harm. Making teach-back a standard part of every discharge is fundamental to preventing hospital readmissions.
Rethinking Patient and Family Education

Let's be honest. Handing a patient a thick folder of paperwork at discharge isn’t education—it's a box-ticking exercise. Real education empowers patients and their families with information they can actually understand and use at home. This is a cornerstone of preventing hospital readmissions, yet it's precisely where so many care plans miss the mark.
Effective education isn't a one-way street. It’s a dynamic conversation that requires us to ditch the medical jargon and connect with people on their level. That means listening more than we talk, inviting questions, and confirming they truly get it. When we do this right, we build the confidence patients need to manage their health once they walk out our doors.
Move Beyond the One-Size-Fits-All Handout
Every patient is different. Their ability to absorb complex health information is shaped by everything from their health literacy and cultural background to their preferred learning style. A strategy that clicks for one person can completely fail with another, leading straight to confusion and non-adherence.
Think about it: a visual learner might get lost in a dense, text-heavy handout but will thrive with a simple chart. Someone with low health literacy could feel intimidated by complex terms, while another patient might want all the technical details. Recognizing these differences is the first step toward creating education that actually sticks.
Simply asking, "Do you have any questions?" just doesn't cut it. The responsibility falls on us, the providers, to present information in a way that’s clear, accessible, and meaningful to each individual patient and their family.
This patient-centered mindset ensures information isn't just delivered, but truly understood. It's vital for a safe recovery.
Make Complex Instructions Simple and Actionable
The secret to great patient education is clarity. We have to break down complicated care plans into simple, manageable steps that feel doable. Bombarding a patient with information is just as counterproductive as giving them none at all.
Here are a few ways we translate complex instructions into real-world actions:
- Medication Schedules: Instead of just a list of drug names and times, create a visual pill chart. Use icons like a sun for morning and a moon for night, complete with pictures of the pills. This is a lifesaver for patients juggling multiple prescriptions.
- Dietary Changes: Don't just hand over a "low-sodium foods" list. Put it in the context of their daily meals. Talk about swapping canned soup for fresh, or using herbs for flavor instead of salt. It’s all about practical, everyday choices.
- Wound Care: For anyone recovering from surgery or an injury, clear wound care instructions are non-negotiable. Verbal directions alone are rarely enough. We have to physically demonstrate the process and back it up with simple, visual guides. Knowing the signs of infection and how to change dressings correctly is critical. In fact, our guide on how to heal deep wounds faster offers clear steps that perfectly reinforce this kind of hands-on education.
This commitment to clarity directly fights one of the biggest drivers of readmissions: confusion.
Create an Interactive Learning Environment
The best education happens when it’s a dialogue, not a monologue. The goal is to create a safe space where patients and their families feel comfortable asking anything—even the questions they worry might sound "silly." There are no silly questions when it comes to someone's health.
Engagement is everything. Instead of talking at them, pull them into the conversation. Ask questions that make them think, like, "Okay, based on what we just discussed, what would you do if you noticed the skin around the wound turning red?" This "teach-back" method helps cement their understanding and build problem-solving skills.
By shifting from passive info-dumping to active, engaged learning, we empower our patients. They leave not just with a piece of paper, but with the knowledge and confidence to follow through, significantly cutting the risk of a return visit. This interactive approach is fundamental to preventing hospital readmissions.
Creating Effective Post-Discharge Follow-Up Systems
The journey to preventing hospital readmissions doesn’t end when a patient walks out the door. In fact, you could argue the most critical phase has just begun. Those first few days at home are a fragile, high-stakes period where small issues can quickly snowball into major complications requiring another hospital stay.
A structured, proactive follow-up system acts as a vital lifeline during this vulnerable time. It's about more than just checking a box; it's about actively engaging with patients to ensure they feel supported, understand their care plan, and know exactly who to call before a problem becomes an emergency. This system is the cornerstone of any serious effort to keep patients recovering safely where they want to be—at home.
The Power of the 48-Hour Follow-Up Call
One of the simplest yet most effective tools in your arsenal is a follow-up call within 48 to 72 hours of discharge. This call is a powerful intervention. It shows the patient you're still invested in their recovery, provides a chance to clarify lingering questions, and helps you spot red flags early on.
The person making this call—whether a nurse, care coordinator, or dedicated team member—needs to be armed with the patient's discharge summary. The goal isn't just to ask, "How are you doing?" but to dig deeper with specific, targeted questions.
A successful follow-up call script might include checks like:
- Medication Review: "Were you able to pick up your new prescriptions? Are you clear on when and how to take each one?"
- Symptom Check: "Are you experiencing any new or worsening symptoms, like increased pain, shortness of breath, or swelling?"
- Appointment Confirmation: "I see you have a follow-up with Dr. Smith next Tuesday. Do you have transportation arranged for that?"
- Problem-Solving: "Is there anything at all making it difficult to follow your care instructions at home?"
This one conversation provides invaluable real-time feedback. You might discover a patient couldn't afford a prescription co-pay or that they misunderstood their dietary restrictions. Catching these issues within the first couple of days allows you to intervene immediately, preventing a potential readmission down the line.
The data below shows just how much impact one part of the discharge plan—medication management—can have on readmission rates.
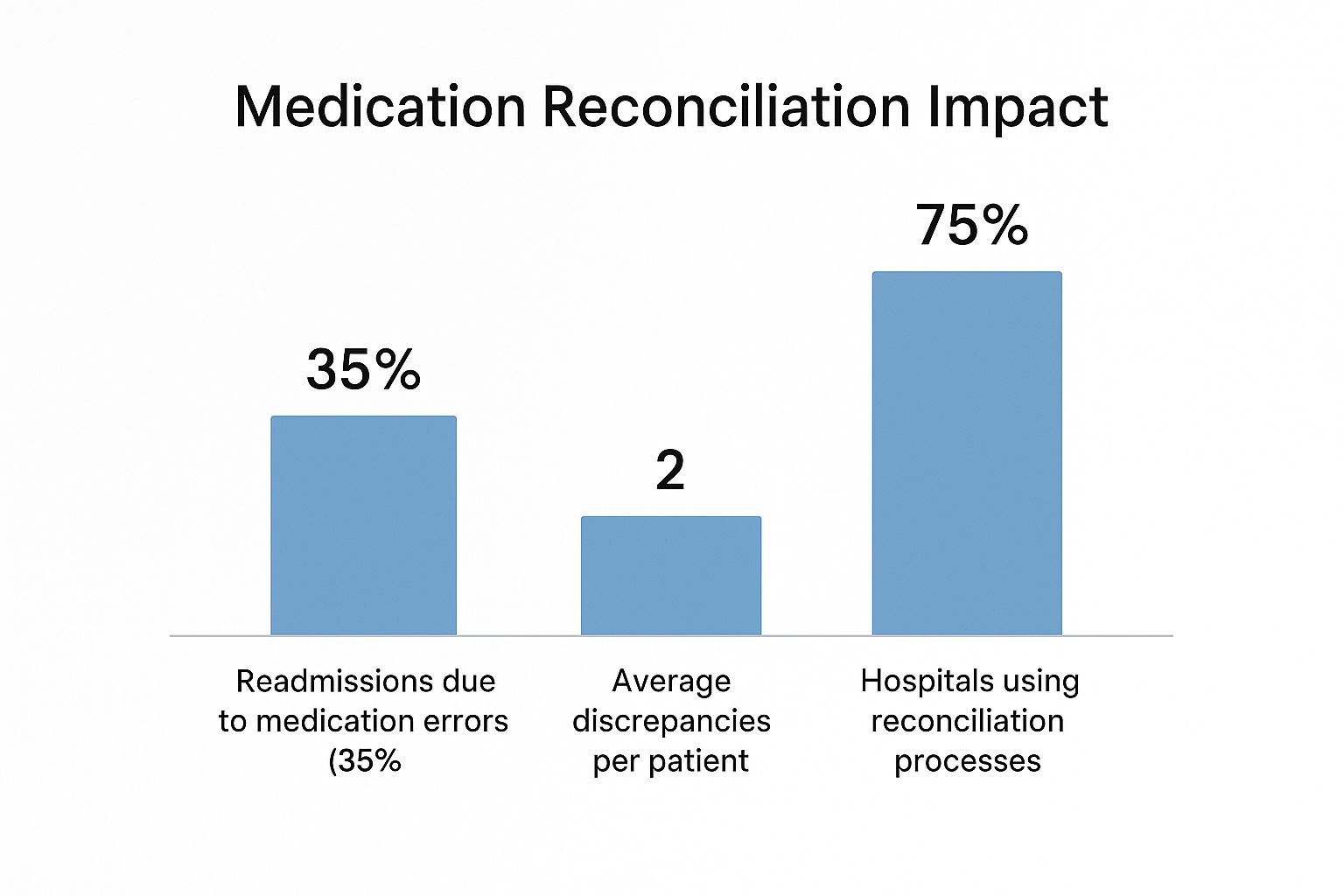
This just goes to show how common medication discrepancies are and underscores why a simple call to confirm a patient's understanding is so critical for keeping them out of the hospital.
Identifying and Supporting High-Risk Patients
Not every patient requires the same level of post-discharge support. A key to an efficient and effective system is segmenting patients by risk. When you identify who is most likely to be readmitted, you can deploy your resources where they’ll have the greatest impact.
Elderly patients, for instance, are disproportionately affected due to complex conditions and social factors. We've seen remarkable success when organizations use data to pinpoint these individuals.
The table below illustrates the power of this targeted approach. By using Clinical Risk Groups (CRGs) to focus their efforts, two different healthcare organizations saw significant drops in costly, adverse events for their highest-risk patients.
Impact of Targeted Interventions on High-Risk Patient Groups
| Intervention Group | Hospital Readmission Reduction | Emergency Department Visit Reduction |
|---|---|---|
| Accountable Care Organization (ACO) | 5.7% | 6.3% |
| State Medicaid Program | 11.5% | 9.8% |
These numbers aren't just statistics; they represent hundreds of patients who avoided a stressful and unnecessary return to the hospital. It's clear that focusing intensive resources on those who need them most is a winning strategy. For these high-risk individuals, a simple phone call may not be enough. This is where more hands-on follow-up strategies come into play.
A tiered approach to follow-up ensures that the most vulnerable patients receive the highest level of support, maximizing your impact without overwhelming your resources. This is smart, patient-centered care.
Your system should be flexible enough to deploy different tools based on the patient's specific needs:
- Telehealth Visits: A virtual check-in can be perfect for a visual assessment, like checking a surgical incision or observing a patient's breathing from afar.
- Home Health Visits: For the highest-risk patients, nothing replaces an in-person visit. A nurse can perform a physical assessment, review medications directly from the pill bottles, and evaluate the home for safety hazards. This is especially crucial for those needing ongoing wound care. Our guide offers more detail on setting up effective post-discharge wound care at home.
By building a robust follow-up system that combines proactive outreach with strategic risk segmentation, you create a powerful safety net. You'll bridge the gap between hospital and home, fundamentally strengthening your strategy to prevent hospital readmissions.
Specialized Strategies for Chronic Conditions

A one-size-fits-all approach to preventing hospital readmissions is almost guaranteed to fail your patients with chronic conditions. Think about it. These individuals, especially those managing complex diseases like heart failure (HF), COPD, or diabetes, are living in a state of delicate balance.
One small slip-up in medication, diet, or symptom tracking can quickly snowball into a full-blown crisis, landing them right back in the hospital.
For these patients, a standard discharge plan just doesn't cut it. They need a more nuanced, continuous level of care that goes far beyond the hospital walls. Real success comes from building specialized strategies that address the unique, day-to-day realities of living with a lifelong illness. This means shifting our mindset from a single discharge event to a model of ongoing management and support.
The Stubborn Challenge of Heart Failure Readmissions
Heart failure consistently ranks as one of the most persistent drivers of hospital readmissions, even as care coordination improves across the board. It's a frustrating reality. A recent analysis of over 6.6 million HF hospitalizations revealed that a staggering 18.2% of patients were readmitted within 30 days.
That number tells a clear story: generic discharge protocols are failing this population. You can dig into the trends in heart failure readmissions yourself to see just how significant this challenge is. These protocols often miss the subtle but critical details of effective HF management.
Establishing Dedicated Support Systems
So, how do we actually move the needle? Many leading health systems are now creating dedicated clinics or focused programs for high-risk chronic conditions. An HF clinic, for instance, can act as a crucial lifeline for recently discharged patients, giving them a level of specialized care that a general primary care office often isn't equipped to provide.
These focused units create the perfect environment for:
- Rapid Follow-Up: Getting patients in the door within days of discharge to assess fluid status and fine-tune medications.
- Expert Education: Providing deep-dive coaching on the tough stuff, like mastering a low-sodium diet and understanding fluid restrictions.
- Seamless Collaboration: Making sure the cardiologist, PCP, and any home health teams are all on the same page, all the time.
For patients with chronic conditions, the goal isn't just to prevent a readmission this month. It’s to empower them with the skills and support to manage their health for a lifetime. This is a long-term partnership, not a one-time fix.
This kind of structure acts as a safety net, catching problems long before they escalate and ensuring patients don’t fall through the cracks as they move between different providers and care settings.
Leveraging Daily Monitoring and Home-Based Care
For many people with chronic conditions, daily self-monitoring is an absolute game-changer. For a heart failure patient, that simple act of stepping on a scale every morning is one of the most powerful tools we have for preventing hospital readmissions.
Why? Because a sudden weight gain of just two or three pounds is a classic early warning sign of fluid retention. That one data point can trigger a quick call to their provider for a medication tweak—often avoiding an ER visit entirely.
This is where technology and hands-on support become indispensable. Remote patient monitoring (RPM) tools can automatically send daily weights and blood pressure readings straight to the clinical team. For patients who need more direct support, skilled professionals visiting the home are invaluable. There are many reasons home health care is essential, and this is a prime example.
A home health nurse doesn't just reinforce education; they can physically assess the patient and their home environment, providing a level of insight you simply can't get in a clinic. It's this proactive, hands-on approach that truly makes the difference.
Your Questions Answered on Preventing Readmissions
Even with the best strategies on paper, preventing hospital readmissions is tough work in the real world. This challenge touches every part of the care journey, from the moment a patient is admitted to the crucial weeks after they’ve gone home.
Let’s dig into some of the most common questions we hear from healthcare teams on the front lines. We'll give you direct, practical answers to help you navigate the hurdles and refine your approach.
What Is the Single Most Effective Strategy?
So many teams are looking for that one "magic bullet" to fix the readmission problem, but honestly, it doesn't exist. The single most powerful approach isn’t one specific action but a system of them all working in concert. A multi-layered, coordinated discharge process is where you'll find the real power.
Think of it like building a safety net. Each thread is a different part of the process, and they all have to be woven together to be strong. It all starts with discharge planning from day one, flows into clear patient education using the "teach-back" method, includes careful medication reconciliation, and is capped off with timely post-discharge follow-up.
This synergy is what creates a solid defense. For example, a patient who has a good "teach-back" session is far more likely to understand their prescriptions. That understanding is then reinforced by a follow-up call within 72 hours to confirm they're taking everything correctly. It’s that combination—prepare the patient, fix medication issues, and provide clear support—that tackles the most common reasons for readmission head-on.
The most powerful strategy isn't a single intervention but the seamless integration of multiple actions. It’s the synergy between patient education, medication safety, and proactive follow-up that truly prevents a return to the hospital.
Each layer reinforces the others, creating a system that’s far stronger than any single piece on its own.
How Can We Address Social Factors That Contribute to Readmissions?
Tackling the social determinants of health (SDOH) means we have to look beyond the hospital's four walls and into the real-world challenges our patients face every day. Things like unstable housing, food insecurity, or a simple lack of transportation can completely derail an otherwise perfect care plan.
The first move is to actually screen for these needs. Simple, non-judgmental questionnaires at admission can quickly flag patients who might struggle after discharge. Once you know who is at risk, the key is having a system in place to connect them with community resources. This is where social workers and dedicated care navigators are absolute heroes.
Here’s what that looks like in practice:
- Transportation Barriers: If a patient can't get to their first crucial follow-up appointment, telling them "it's important" isn't enough. You have to actively arrange non-emergency medical transport or link them with a local volunteer driver program.
- Food Insecurity: For someone with heart failure or diabetes on a strict diet, not having access to healthy food is a huge readmission risk. The fix is a direct referral to a food bank, a Meals on Wheels program, or a local "food as medicine" initiative.
Building strong partnerships with these community organizations is non-negotiable. It creates a genuine support network that addresses the root social causes of poor health, making a safe recovery at home truly achievable.
What Role Does Technology Play in Reducing Readmissions?
Technology is a massive force multiplier here, helping our teams work smarter, not just harder. It’s an indispensable tool for bridging gaps in communication and monitoring that so often lead to readmissions.
For instance, modern electronic health records (EHRs) can use predictive analytics to automatically flag high-risk patients. This lets teams focus their intensive efforts where they're needed most, instead of using a one-size-fits-all approach. Telehealth has also become a game-changer, making post-discharge check-ins so much more accessible, especially for patients with mobility issues or those in rural areas.
Even better, remote patient monitoring (RPM) tools give us a direct window into a patient's daily health. A connected scale for a heart failure patient or a glucose monitor for someone with diabetes can send real-time data back to the clinical team. This allows for intervention at the very first sign of trouble—often before the patient even feels symptoms. A small, sudden weight gain can be addressed with a quick medication tweak, heading off a major fluid overload event. This proactive management is especially critical for complex wound care cases. You can see how this works by exploring what mobile wound care is and why it is important.
How Can We Implement These Strategies Without Overwhelming Our Team?
Introducing new workflows to a team that’s already stretched thin is a legitimate concern. The secret is to focus on efficiency, clearly defined roles, and smart automation. Don't try to boil the ocean. Start small and build momentum.
Kick things off with a pilot program. Focus on a single, high-risk patient group, like those with COPD. This lets you test and fine-tune your process on a manageable scale before attempting a hospital-wide rollout.
Most importantly, define roles and share the load.
- Let nurses own the "teach-back" education at the bedside. They’re the best at it.
- Have care coordinators manage the logistics—scheduling follow-ups and arranging transport.
- Put pharmacists in charge of leading the medication reconciliation process.
Building standardized checklists right into your EHR can also make a world of difference. These tools guide the team, reduce the mental load, and make sure no critical steps get missed. Finally, use technology to automate simple, repetitive work like sending appointment reminders via text. This frees up your skilled team to focus on the high-touch, high-value work that only people can do. The upfront effort to create these efficient systems pays off, not just in better outcomes but also in team morale when they see the incredible impact of their work.
At Rapid Wound Care, we understand the critical importance of strong post-discharge support in preventing readmissions. Our specialized at-home services ensure patients receive the expert care they need to heal properly and avoid complications. Learn how our dedicated team can become a vital part of your readmission reduction strategy by visiting us at https://rapidwoundcare.com.

