What you do in the first 24 hours after an injury is absolutely crucial. It sets the entire tone for your body’s recovery, determining whether healing will be quick and straightforward or slow and complicated. Your immediate actions can either create the perfect healing environment or get in the way of your body's natural repair crew.
Your First 24 Hours for Optimal Healing

When you get a minor cut or scrape, your first instinct might be to douse it with the harshest antiseptic you can find. But in my experience, creating the right environment for healing is more about gentle support than aggressive cleaning. Those initial moments are your best shot at preventing infection and giving your body a major head start.
The Right Way to Clean a Wound
Before you even touch the wound, wash your hands thoroughly. That’s step zero.
Then, it's time to clean the wound itself. I know what you’re thinking—bring on the stinging hydrogen peroxide or rubbing alcohol. But please don’t. These substances are cytotoxic, which is a fancy way of saying they kill cells. They don’t just kill bacteria; they destroy the delicate new tissue your body is working hard to build, which can ironically slow down the very healing you're trying to achieve.
A gentle approach works so much better. Just wash the area with cool or lukewarm running water and a mild soap. Your goal here is simple: flush out any dirt, debris, or bacteria without causing more damage to the surrounding skin. Once it's clean, gently pat the area dry with a sterile gauze pad or a clean cloth.
Key Takeaway: Mild soap and water are your best friends for cleaning a new wound. Harsh antiseptics like hydrogen peroxide can actually harm new tissue and delay recovery.
Embrace Moist Wound Healing
The old advice to “let a wound air out” so it can form a scab? That's officially outdated. Years of research and clinical practice have shown us that wounds heal faster, and with less scarring, when they're kept in a moist, covered environment.
When a wound dries out, it forms a hard, thick scab. Think of that scab as a roadblock. It makes it much more difficult for new skin cells to travel across the wound bed and close the gap.
Keeping the wound properly moist with a good dressing helps you hit several key goals for faster healing:
- It protects new cells by keeping them hydrated and alive so they can do their job.
- It prevents a hard scab from forming, creating a clear path for new tissue.
- It reduces infection risk by acting as a physical shield against outside bacteria.
A thin layer of an over-the-counter antibiotic ointment can help create this moist environment. Cover it with a sterile bandage or dressing. This one simple step is probably the most impactful thing you can do in that first 24-hour window.
For anyone managing wounds at home long-term, mastering these basic techniques is non-negotiable. We cover this and more in our guide on effective post-discharge wound care at home.
Just remember to change the dressing at least once a day—or more often if it gets wet or dirty—to keep the healing environment clean and effective.
Fueling Your Recovery Through Nutrition

While the right dressing and external care set the stage for healing, true recovery is an inside job. The food and fluids you consume are the raw materials your body needs to rebuild tissue, fight off infection, and repair itself from the inside out.
Think of your body as a construction site. Without a steady supply of bricks, mortar, and fuel, the whole project grinds to a halt. When it comes to healing a wound, your diet is that critical supply chain. This isn't just about "eating healthy"—it's about strategically giving your body the specific nutrients it's screaming for during this high-stress period.
Every meal is an opportunity to either speed up or slow down your recovery.
The Power of Protein
Protein is the undisputed king of tissue repair. It provides the essential amino acids that act as the fundamental building blocks for new skin, blood vessels, and muscle. It's no surprise that during the healing process, your body's protein needs can skyrocket.
A breakfast smoothie, for instance, can be more than just a quick meal; it can be a healing powerhouse. Try blending Greek yogurt (an amazing source of protein) with a handful of spinach and a scoop of quality protein powder. This simple drink delivers the foundational materials your cells need to get to work.
Other fantastic protein sources include:
- Lean meats like chicken and turkey
- Fatty fish like salmon, which also deliver anti-inflammatory omega-3s
- Eggs, beans, and lentils
- Tofu and other soy-based products
A pro tip I always share with my patients: include a source of protein with every single meal and snack. This creates a constant, steady supply of amino acids for your body to draw from, rather than one big dose it can't fully use at once.
Vitamins and Minerals Your Wound Demands
If protein is the foundation, think of specific vitamins and minerals as the skilled crew, directing the repair process and making sure everything comes together correctly. Two of the most important players on this team are Vitamin C and Zinc.
Vitamin C is absolutely critical for synthesizing collagen, the main structural protein in our skin. Without enough Vitamin C, your body simply cannot produce strong, healthy new tissue. You'll find it in abundance in citrus fruits, bell peppers, broccoli, and strawberries.
Zinc plays a huge part in cell growth and immune function. A zinc deficiency can directly stall wound healing by slowing down the creation of new skin cells. To boost your intake, focus on foods like nuts, seeds, whole grains, and lean red meat.
A perfect example of a healing-focused meal would be lunch with grilled salmon (protein and omega-3s), a side of roasted broccoli (Vitamin C), and a scoop of quinoa (protein and zinc). When dealing with more significant injuries, these nutritional strategies become even more vital. You can learn more about how to support your body to heal deep wounds faster with our comprehensive guide.
The Critical Role of Hydration
Perhaps the most overlooked, yet simplest, key to recovery is water. Your blood, which is responsible for carrying oxygen and all these vital nutrients to the wound site, is mostly water. Simple as that.
Even slight dehydration can thicken the blood, making this delivery system sluggish and inefficient. When nutrient transport slows, healing slows right along with it. You're essentially starving your new cells of the resources they need to thrive.
Aim to sip water consistently throughout the day—don't wait until you feel thirsty. A good target is eight 8-ounce glasses, but your personal needs might be higher. An easy way to check is to look at your urine color. If it’s pale straw, you're on the right track. Dark yellow? Your body is sending a clear signal for more fluids. Staying hydrated is one of the most effective things you can do to support your body’s natural healing power.
The Evolution of Modern Wound Dressings
Wound care has come a long way from the basic adhesive strips and gauze pads most of us grew up with. Today’s advanced dressings aren’t just passive covers; they are active, intelligent tools designed to work with your body's natural healing process.
Think of them as creating the perfect microenvironment for repair. This shift from simply covering a wound to actively managing it is one of the biggest leaps forward in achieving faster, more effective healing, especially for serious or slow-to-heal injuries.
The right dressing can do more than just block bacteria. It can manage moisture, encourage new tissue to form, and dramatically shorten recovery timelines. This chart breaks down just how much of a difference modern wound care can make.
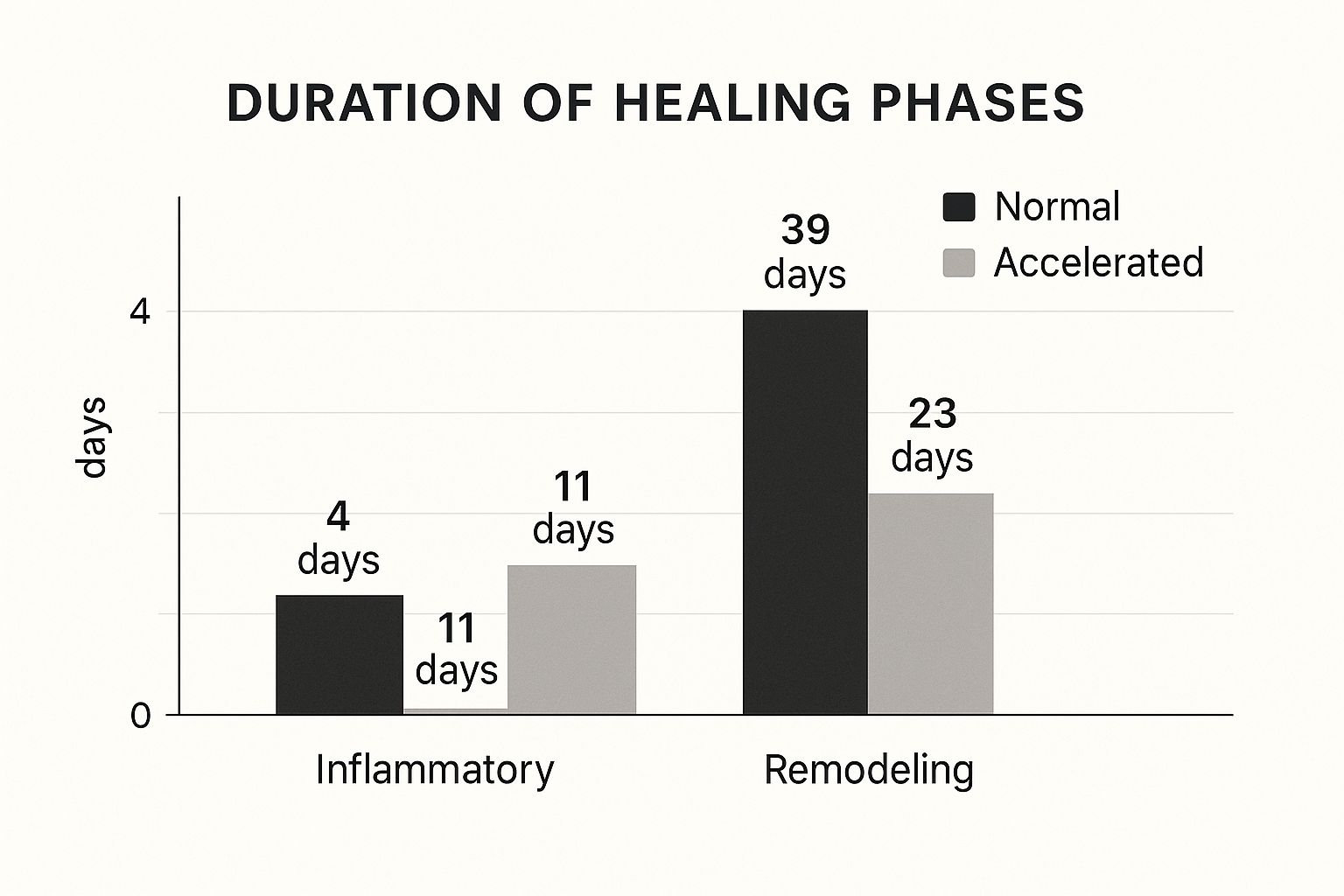
As you can see, optimizing each stage of healing isn’t just a small improvement—it can slash total recovery time.
Beyond Basic Bandages
The core principle behind all modern dressings is moist wound healing. The old advice to “let a wound air out” actually slows things down by creating a hard, dry scab. We now know that keeping a wound properly hydrated allows new skin cells to move freely across the surface and close the gap much more efficiently.
This is a huge departure from outdated methods like wet-to-dry dressings. While once used to clean wounds, this technique was often painful and could rip away healthy new cells during removal. You can learn more about the drawbacks of wet-to-dry wound care dressing changes and why they've been replaced by gentler, more effective options.
Meet the Modern Dressing Family
Today, we have a whole family of advanced dressings, each designed for specific types of wounds and healing stages. Knowing the difference can help you have a much more productive conversation with your doctor or wound care specialist.
This growing demand for better solutions is driving major growth in the healthcare market. The global wound care industry was valued at roughly USD 24.08 billion in 2025 and is expected to hit USD 29.57 billion by 2030. This investment means more innovation and better products are constantly becoming available.
To make sense of the options, here’s a quick comparison of some of the most common advanced dressings used today.
Modern Wound Dressing Comparison
| Dressing Type | Best For | Key Benefit |
|---|---|---|
| Hydrocolloid | Clean, non-infected wounds with low drainage (e.g., minor burns, pressure sores) | Creates a moist, insulating, and protective gel barrier. |
| Foam | Wounds with moderate to heavy fluid (exudate) | Highly absorbent and cushioning, keeps wound moist without soaking skin. |
| Alginate | Wounds with significant drainage | Made from seaweed; forms a gel to trap bacteria and absorb large fluid amounts. |
| Hydrogel | Dry or dehydrated wounds with little to no drainage (e.g., certain burns, ulcers) | Donates moisture to the wound bed to rehydrate it and promote healing. |
Understanding these categories helps illustrate that modern wound care is highly specific, aiming to provide exactly what a particular wound needs to heal.
Key Insight: The goal of a modern dressing is to maintain a perfect moisture balance—not too wet, not too dry. This "Goldilocks" environment is the sweet spot where cells thrive and healing takes off.
Choosing the Right Dressing for the Job
Selecting the right dressing is never a one-size-fits-all situation. The decision hinges entirely on the wound’s characteristics: its location, size, depth, and how much fluid it’s producing.
For instance, a shallow scrape on your knee might heal perfectly with a simple hydrocolloid patch. A deeper, more serious wound with heavy drainage, however, would demand a more absorbent foam or alginate dressing to manage the fluid and prevent complications.
Using the wrong product can actually set you back. Putting a super-absorbent dressing on a dry wound will dehydrate it and stall healing. On the flip side, using a non-absorbent dressing on a wet wound can trap moisture, damage the surrounding skin, and create a breeding ground for infection. This is precisely why professional guidance is critical for anything beyond a minor cut or scrape.
Turning to Nature for Bioactive Healing

While advanced dressings and good nutrition are the bedrock of modern wound care, sometimes the most powerful allies come straight from nature. For centuries, people have used certain plants and natural substances to soothe injuries. It turns out, they were onto something.
Today, science is catching up to what traditional medicine has practiced for generations. We now know that some of these compounds don’t just sit on top of a wound—they’re bioactive, meaning they actively take part in the healing process.
These natural agents can fight off bacteria, calm inflammation, and even give your own cells a nudge to work harder. Folding them into your wound care routine can provide a gentle but surprisingly effective boost, helping your body do what it does best: repair itself.
The Science Behind Nature's Healers
Of course, not every folk remedy holds up under a microscope. It’s crucial to stick with the ones that have solid science behind them. Two of the most respected and well-researched natural agents are medical-grade honey and aloe vera.
You have to be specific here—we're talking about medical-grade honey, particularly Manuka honey, which is a world away from the stuff you put in your tea. This honey has powerful antimicrobial properties that make it tough for bacteria to survive. Its high sugar content pulls moisture right out of bacterial cells, and its low pH creates an acidic environment that stops germs in their tracks. It’s an amazing way to create a protective, moist barrier that also actively cleans the wound.
Then there’s aloe vera, the superstar of soothing. Famous for its anti-inflammatory effects, the gel from an aloe plant is a go-to for minor burns and skin irritations because it helps dial down pain and redness. It contains compounds that improve circulation and slow the growth of certain bacteria, creating a much better environment for healing.
Key Takeaway: Bioactive ingredients from nature are more than just a cover-up. They are active participants in healing—fighting bacteria, reducing inflammation, and encouraging new, healthy tissue to grow.
Emerging Natural Compounds on the Horizon
The search for nature’s next super-healer is always on. Researchers are constantly exploring new ways to use the plant world in modern medicine, and one of the most exciting frontiers is integrating plant extracts directly into advanced wound dressings.
A perfect example is the work being done with Moringa oleifera, a plant that has been used on skin sores for ages. Recent scientific studies are confirming its potential. Extracts from M. oleifera leaves have been found to significantly speed up cell migration and proliferation—two critical steps in closing a wound. This kind of research, like a study you can read about on the University of Bath’s research portal, is paving the way for a new generation of treatments.
This blend of ancient wisdom and modern science is opening up new possibilities for treatments that are both incredibly effective and gentle on the body.
Practical Tips for Using Natural Agents Safely
If you’re thinking about trying natural options, it's vital to do it right. A little common sense goes a long way.
- Always Go for Medical-Grade: This is non-negotiable for honey. Never, ever put honey from the grocery store on an open wound. It isn’t sterilized and can contain harmful bacterial spores. Stick to products specifically designed and sterilized for medical use.
- Do a Patch Test First: Before you apply anything new to a wound, test a small amount on an unbroken patch of skin nearby. You’re looking for any signs of an allergic reaction or irritation.
- Know Your Limits: Natural agents are fantastic for minor cuts, scrapes, and burns. But for anything deep, large, or showing signs of infection, you need to see a professional. No exceptions.
By understanding the real, science-backed benefits of these natural compounds, you can make smarter choices for your care. Leaning on nature’s pharmacy can be a smart and supportive step toward a faster, smoother recovery.
How Age and Health Impact Your Recovery
Wound healing is never a one-size-fits-all journey. Your body's ability to repair itself is deeply intertwined with your age and overall health. A simple cut that might vanish in a few days on a teenager could linger for weeks on an older adult, and it’s critical to understand the reasons why.
As we age, our internal repair crews naturally slow down. Skin loses some of its thickness and elasticity, and our immune response just isn't as quick on the draw as it used to be. This means the body’s first responders—the cells that fight off infection and kickstart the rebuilding process—don’t arrive at the wound site as quickly or work with the same efficiency.
This isn't just an individual concern; it's a global one. The world's population is getting older, and this demographic shift is a major driver for better wound care solutions. The World Health Organization projects that by 2030, one in every six people will be 60 or older. This matters immensely because as this population grows, so does the need for effective healing strategies, especially in markets like the United States, which already accounts for over 45% of the demand for global wound care products.
When Chronic Conditions Complicate Healing
Beyond age, certain chronic health conditions can throw up major roadblocks on the path to recovery. They disrupt the very systems your body relies on for repair, capable of turning a minor injury into a serious, long-term medical challenge.
Diabetes is one of the biggest culprits. Persistently high blood sugar levels can wreak havoc on nerves, especially in the feet—a condition called neuropathy. When you can't feel a small cut, blister, or pressure spot, it can go completely unnoticed until it develops into a severe sore, known as a diabetic foot ulcer.
On top of that, diabetes often impairs circulation. Imagine your circulatory system as a superhighway delivering oxygen, nutrients, and healing factors to the wound. Poor circulation clogs that highway, preventing those essential building materials from ever reaching their destination.
Expert Insight: For anyone with diabetes, a wound is never just skin-deep; it’s a reflection of a systemic issue. Keeping blood sugar in check isn't just part of managing diabetes—it's one of the most critical parts of wound care.
Other conditions that can seriously slam the brakes on recovery include:
- Peripheral Artery Disease (PAD): This condition narrows the arteries, starving the limbs of the oxygen-rich blood that wounds desperately need to heal.
- Venous Insufficiency: When veins in the legs struggle to push blood back to the heart, it can pool, causing swelling, pressure, and skin breakdown.
- Weakened Immune System: Any condition that compromises immunity leaves a wound wide open to infections that can quickly derail the entire healing process.
Proactive Strategies for Overcoming These Hurdles
If you're dealing with age-related delays or a chronic condition, it doesn't mean you're doomed to poor healing. It just means you have to be more vigilant and proactive. The best approach is always a combination of smart self-care and professional expertise.
First and foremost, managing your underlying health condition is the most powerful move you can make. If you have diabetes, that means diligent blood sugar monitoring. If you have PAD, it could involve lifestyle changes and medications to get your circulation flowing better.
Daily wound monitoring also becomes absolutely non-negotiable. You have to be your own first line of defense. Check your wound every single day for any red flags:
- Spreading Redness: Is the redness moving away from the wound's edges?
- Unusual Drainage: Do you see any yellow or green pus? Is there a foul odor?
- Worsening Pain: Is the wound becoming more painful over time instead of less?
- Excessive Swelling: Is the area around the injury puffy, tight, or swollen?
Noticing any of these signs is your cue to call a healthcare professional immediately. Don't wait.
The Power of Specialized Care
For wounds that are stubborn and slow to heal, specialized care can be a total game-changer. This is where at-home wound care services prove their worth, bringing expert treatment right to your doorstep. For anyone with mobility challenges, this approach eliminates the stress and physical burden of traveling to a clinic.
A wound care specialist offers advanced treatments that go far beyond basic first aid. They can properly clean and dress complex wounds, manage stubborn infections, and create a care plan tailored specifically to you and your health challenges. This focused, expert attention is often the key to finally getting on the path to recovery. To see what this looks like in the real world, check out our guide on how home wound care speeds up recovery.
By taking control of your health and bringing in the right support, you can help your body overcome these hurdles and heal faster.
Common Questions About Healing Wounds
When you're trying to heal, it's easy to get bogged down by confusing advice. There's a lot of misinformation out there, and plenty of old wives' tales about wound care still make the rounds. Getting clear, science-backed answers is the best way to speed up your recovery and feel confident you're doing the right thing.
Let's cut through the noise and tackle some of the most common questions I hear from patients.
Should I Let a Wound Air Out to Heal Faster?
This is probably the most persistent myth in wound care, but the answer is a hard no. I know it feels intuitive to "air out" a cut or scrape, but modern wound science tells us this actually slows things down.
When a wound is left open to the air, it dries out and forms a thick, hard scab. That scab might seem like a good thing, but it’s really a barrier. It makes it much harder for new skin cells to travel across the wound bed and close the gap.
The Modern Approach: A moist, covered environment is the gold standard for cell regeneration and faster healing. A clean, breathable bandage creates the perfect runway for new skin growth, protecting the delicate tissue from bacteria while preventing a hard scab from forming.
Just be sure to change the dressing at least once a day, or any time it gets wet or dirty, to keep the area clean and primed for healing.
What Are the Signs My Wound Is Not Healing Properly?
Knowing the red flags of a wound in trouble is one of the most important things you can learn. A little initial redness, some swelling, and even a bit of clear fluid are all normal parts of the healing cascade. But certain signs tell you it's time to call a professional.
Keep an eye out for these key warning signs of a potential infection or complication:
- Redness that starts spreading away from the wound’s edges.
- Pain that gets worse over time instead of better.
- Thick, cloudy, yellow, or green discharge from the wound.
- Any kind of foul or unpleasant odor.
- Feeling feverish, shivery, or generally unwell.
If you spot any of these signs, don't just wait and see. It’s time to get in touch with a healthcare provider right away for an evaluation.
Is It Safe to Use Hydrogen Peroxide to Clean a Wound?
Here's another outdated practice that has thankfully fallen out of favor. For routine wound care, we no longer recommend using aggressive antiseptics like hydrogen peroxide or rubbing alcohol.
Sure, these liquids are great at killing bacteria, but they’re also cytotoxic—which is a technical way of saying they're toxic to your cells. They can't tell the difference between harmful germs and the fragile, healthy new cells your body is working so hard to build. This cellular damage can seriously set back your healing timeline.
For most minor cuts and scrapes, the best approach is gentle cleansing with mild soap and clean, running water. That’s all you need to effectively remove debris without harming the new tissue. Of course, the best way to clean a wound can depend on what caused it, so it's always helpful to understand the 6 types of wounds to better inform your care.
How Much Does Stress Really Affect Healing?
The mind-body connection is incredibly powerful, and stress has a real, measurable impact on how well your body can repair itself. When you’re under high levels of chronic stress, your body pumps out hormones like cortisol.
This isn't just a feeling—it's a physiological response. Cortisol suppresses your immune system and cranks up inflammation throughout your body, which directly interferes with the finely tuned stages of wound repair. It essentially puts the brakes on your recovery.
Finding simple ways to manage stress can make a huge difference. Things like deep breathing exercises, making sure you get enough sleep, and even light physical activity (once your doctor gives you the green light) can help lower cortisol and give your body the support it needs to heal.

