Understanding Wound Infection: A 2025 Guide
This guide details the signs of infected wound, helping you quickly identify potential problems and seek appropriate care. Knowing these signs is crucial for preventing serious complications and promoting healing. Whether you're a patient, caregiver, or healthcare professional, understanding these indicators empowers you to manage wounds effectively. This list covers key signs like increased pain, pus, redness, swelling, and more. Learn to recognize an infected wound and take timely action.
1. Increased Pain or Tenderness
One of the most significant signs of an infected wound is increased pain or tenderness. While some discomfort is a normal part of the healing process, a wound that becomes more painful over time signals a potential problem. This escalating pain is a critical indicator that should not be ignored, especially as it often precedes visible signs of infection. Understanding the nuances of wound pain and how it relates to infection is crucial for both patients and healthcare providers in ensuring prompt and effective treatment. This heightened sensitivity and discomfort serves as a body's natural alarm system, alerting you to a potential issue that requires attention. For patients managing chronic or acute wounds, recognizing this early sign of infection can significantly impact healing outcomes and prevent serious complications.

Normally, wound pain gradually decreases as healing progresses. In contrast, an infected wound exhibits a reverse trend, with pain intensifying rather than subsiding. This heightened pain results from the body's inflammatory response to the infection. The immune system sends white blood cells to fight the invading bacteria, leading to swelling, heat, and increased sensitivity in the affected area. This inflammatory process, while essential for fighting infection, also contributes to the experience of pain. Several specific features can help distinguish infection-related pain from normal healing discomfort. These include a throbbing or pulsating sensation at the wound site, pain disproportionate to the wound's size, tenderness extending beyond the wound margins, and pain that interferes with sleep or daily activities.
For example, a post-surgical incision that becomes progressively more painful after the initial two or three days could indicate an infection. Similarly, a minor cut that develops throbbing pain instead of gradually healing should raise concern. In individuals with diabetic foot ulcers, escalating pain levels are a serious warning sign that requires immediate medical attention. These examples highlight the importance of recognizing increasing pain as a potential indicator of infection across a range of wound types, from surgical incisions to chronic ulcers. Early detection and treatment are critical, especially for vulnerable populations like those with diabetes, who are at higher risk of developing serious complications from infected wounds.
Monitoring wound pain is a simple yet powerful tool for both patients and caregivers. One effective method is keeping a pain diary, rating the pain on a scale of 1 to 10 each day. This allows for tracking pain trends over time and identifying any increases that may suggest infection. It's also important to note when pain medications become less effective, as this could signify a worsening infection. Paying attention to pain that wakes you from sleep is another crucial indicator, as infection-related pain can be particularly intense at night. Distinguishing between sharp, shooting pain (often associated with nerve damage) and dull, aching pain (more characteristic of infection) can also provide valuable information.
While increased pain is a valuable indicator of a potential wound infection, it is important to acknowledge its limitations. Pain tolerance varies significantly between individuals, meaning what one person perceives as severe pain, another might consider mild discomfort. This subjectivity can make it challenging to assess wound pain objectively. Furthermore, pain medications can mask the underlying pain of an infection, delaying diagnosis. Finally, the discomfort associated with normal wound healing can sometimes be mistaken for infection-related pain, especially in the early stages of recovery. Despite these limitations, increased pain or tenderness remains a crucial early warning sign of infection. When combined with other indicators, such as changes in wound appearance, drainage, or odor, it provides valuable information for guiding treatment decisions. By understanding the characteristics of infection-related pain and employing strategies to monitor pain effectively, patients and healthcare providers can work together to ensure timely intervention and promote optimal wound healing. Recognizing increasing pain as a key sign of infected wound contributes significantly to early diagnosis and appropriate medical intervention, minimizing potential complications and improving overall healing outcomes. For chronic wound sufferers and elderly patients, this vigilance can significantly improve their quality of life and prevent serious health consequences. Early detection and treatment are particularly important for these vulnerable populations.
2. Purulent Discharge (Pus Formation)
One of the most noticeable and concerning signs of an infected wound is the presence of purulent discharge, commonly known as pus. This thick, opaque fluid is a key indicator of a bacterial infection actively battling your body's defenses within the wound bed. While healthy wounds may exhibit some clear or slightly bloody drainage as part of the natural healing process, thick, colored discharge signals a different story. Understanding the characteristics of purulent discharge empowers you to recognize a potential infection early and seek appropriate medical attention. This is crucial for preventing complications and promoting timely healing, particularly for individuals with chronic conditions like diabetes or those in long-term care facilities.
Pus formation is a direct consequence of your body's immune response to bacterial invasion. When bacteria enter a wound, white blood cells, specifically neutrophils, rush to the site to engulf and destroy the invaders. This process creates a battlefield of dead white blood cells, bacteria, and tissue debris, which collectively form the viscous substance we recognize as pus. The color and consistency of pus can vary depending on the type of bacteria involved and the stage of infection.
Several key features distinguish purulent discharge from normal wound exudate: a thick, creamy consistency resembling custard or toothpaste; a coloration ranging from yellow and green to gray or even brown; and often, a foul or unusual odor. Healthy wound drainage, on the other hand, is typically thin and clear or slightly tinged with blood. As the infection progresses, the volume of purulent discharge may increase, and you might observe streaks of blood within it. For patients with chronic wounds, such as diabetic foot ulcers, recognizing these changes is vital for preventing serious complications. Learn more about Purulent Discharge (Pus Formation) This link provides further information specifically related to diabetic foot ulcers and their treatment.
The presence of purulent discharge is a highly specific indicator of a bacterial infection. Its visibility makes it relatively easy for patients, primary care providers, and wound care specialists to recognize. Furthermore, a sample of the discharge can be cultured in a laboratory to pinpoint the specific bacteria causing the infection, which helps guide appropriate antibiotic therapy. This is especially valuable in complex wound cases or for patients with compromised immune systems.
However, purulent discharge may not always appear in the very early stages of infection. Small amounts can sometimes be masked within the wound bed, delaying detection. Additionally, the appearance of pus can sometimes be mistaken for other types of wound exudate, particularly in chronic wounds. The amount of discharge also varies significantly based on the wound's location, size, and depth. A small, superficial wound may produce minimal pus, while a larger, deeper wound could generate a substantial amount.
For patients and caregivers, daily monitoring of wound drainage is essential. Note the color, consistency, and approximate amount of discharge each day, ideally using clean gauze to gently dab the wound and assess the drainage. Any changes in odor or appearance should be documented and reported to a healthcare professional. Avoid squeezing or manually expressing pus, as this can spread the infection to deeper tissues or surrounding skin.
Examples of purulent discharge include thick yellow pus emanating from an infected piercing, green and foul-smelling drainage from a post-operative wound, or white/yellow pus from an infected acne lesion. In the context of chronic wound care, such as with diabetic foot ulcers, the presence of pus often signals the need for more aggressive treatment, possibly including debridement, specialized dressings, and systemic antibiotics. Early identification and appropriate management of purulent discharge are essential for preventing serious complications like sepsis and promoting effective wound healing.
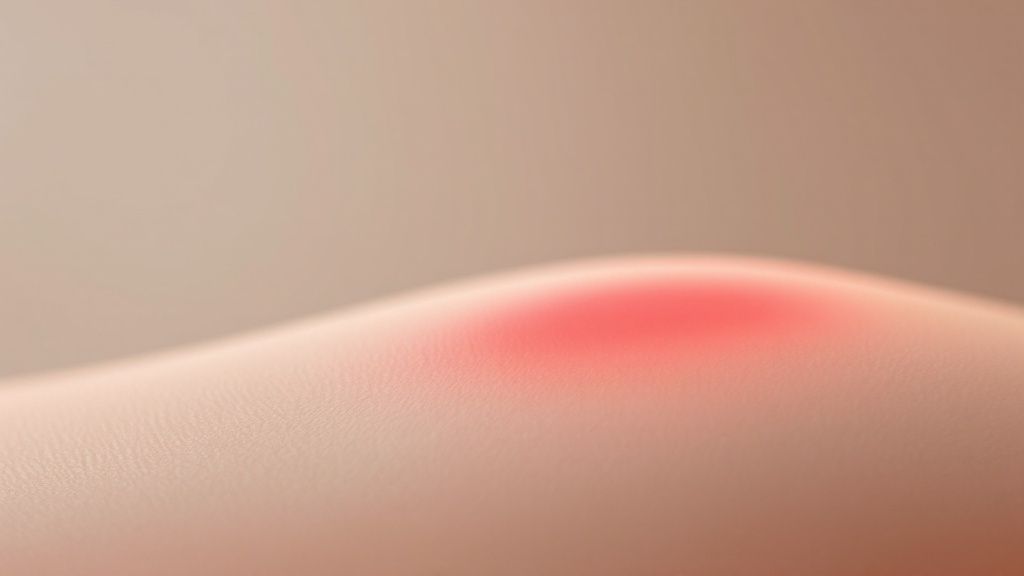
3. Erythema (Redness) Spreading Beyond Wound Edges
One of the most telling signs of an infected wound is the presence of erythema, or redness, that extends beyond the wound's original margins. While a degree of redness directly surrounding a fresh wound is a normal part of the initial inflammatory process, expanding redness is a significant indicator that the infection may be spreading into the surrounding tissues. This occurs as the body's immune system attempts to combat the invading bacteria. The immune response triggers vasodilation, widening blood vessels to bring more white blood cells and other immune components to the affected area. This increased blood flow results in the visible redness characteristic of erythema. Monitoring this redness is crucial for early detection and intervention.

Erythema associated with a wound infection typically presents as a well-defined area of redness expanding outward from the wound edges. This expansion can progress over hours or even days, making regular monitoring critical. The advancing edge of the redness is often distinct, and the affected area may feel warm to the touch due to the increased blood flow. In some cases, the redness may appear as streaks following the lymphatic vessels, which are part of the body’s drainage system and a common pathway for infection spread. These red streaks are a particularly concerning sign and warrant immediate medical attention.
Several features distinguish infection-related erythema from normal wound healing redness. Primarily, it's the spread that sets it apart. Normal inflammatory redness tends to remain localized and diminish as the wound heals. Conversely, the redness caused by infection progressively expands beyond the original wound boundary. Observing and documenting the extent of redness over time is crucial for early recognition of a developing infection.
This visual cue is an invaluable early warning sign of spreading infection, especially for signs of infected wound. Its readily observable nature makes it easy to monitor and measure progression, providing valuable information for healthcare professionals in determining the appropriate course of treatment. The presence of expanding erythema often indicates the need for systemic antibiotic treatment to combat the infection and prevent further complications.
However, assessing erythema does present some challenges. It can be subtle and harder to detect in individuals with darker skin tones. It can also be mistaken for the normal inflammatory response that accompanies wound healing, particularly in the early stages. Furthermore, existing skin conditions can make it difficult to accurately assess the presence and extent of erythema.
Here are some practical tips for monitoring erythema around a wound:
- Mark the edge of redness: Use a pen to carefully outline the visible border of redness. This provides a baseline for comparison and allows you to easily track any expansion.
- Measure and document the diameter daily: Using a ruler, measure the diameter of the reddened area and record it along with the date and time. This provides quantifiable data to track the progression or regression of the erythema.
- Look for red streaking lines: Carefully inspect the area around the wound for any thin, red lines extending away from the wound site, especially towards the heart. These streaks can indicate lymphatic involvement and require immediate medical attention.
- Compare with the unaffected side: If the wound is on a limb or other paired body part, compare it with the opposite side to discern differences in color and temperature.
The video above provides a visual demonstration of how to assess wound erythema. This visual guide can be beneficial for both patients and healthcare providers in identifying the signs of an infected wound.
Recognizing and monitoring erythema is crucial in managing wound care. It allows for timely intervention, prevents complications, and promotes effective healing. By understanding the characteristics of infection-related erythema and following these simple monitoring techniques, patients and caregivers can play a vital role in identifying and managing wound infections effectively. While erythema is a valuable indicator, it's essential to remember that it's just one piece of the puzzle. Always consult with a healthcare professional for any concerns about wound healing or potential infections. They can provide a comprehensive assessment and recommend the appropriate treatment plan.
4. Local Warmth and Heat
One of the most easily detectable signs of a wound infection is localized warmth and heat emanating from the affected area. This symptom arises from the body's natural inflammatory response to harmful bacteria. When a wound becomes infected, the immune system springs into action, sending white blood cells to fight the invading pathogens. This increased blood flow to the site, coupled with the release of inflammatory mediators, results in a noticeable temperature increase in and around the wound. This heat is often one of the cardinal signs of infection and inflammation, making it a crucial indicator for patients and healthcare professionals alike. Detecting this warmth is a vital step in identifying a potential infection and initiating timely treatment.

The sensation of warmth around a wound can range from a mild increase in temperature to a significant, almost burning feeling. The affected area may feel noticeably warmer to the touch compared to the surrounding healthy skin. This temperature difference is a key characteristic of local warmth associated with infection. Often, the warmth extends beyond the immediate wound area, indicating the spread of inflammation. This expansion of the heated area can signal the progression of the infection and should be monitored closely. Persistent heat that doesn't decrease over time is another red flag, suggesting the infection is not resolving on its own. In some cases, this localized heat may be accompanied by a throbbing sensation, further indicating the presence of an active infection. More objectively, the temperature difference can be measured with an infrared thermometer, providing a quantifiable measure of the inflammation.
Several features distinguish infection-related warmth from normal healing processes. While some warmth is expected during the initial stages of wound healing, this typically subsides as the wound closes. Persistent or increasing warmth, especially beyond the immediate wound area, warrants further investigation. The characteristics of local warmth as a sign of infected wound include a noticeable temperature difference, warmth extending beyond the wound, persistent heat, a potential throbbing sensation, and the ability to be measured with an infrared thermometer. These features help differentiate between normal inflammation during healing and an infection.
The ability to detect warmth early on, even before visual changes like redness or pus appear, makes this a valuable diagnostic tool. It allows for early intervention, which can significantly improve treatment outcomes. For example, an infected diabetic foot ulcer may feel hot to the touch before significant visual changes occur. Similarly, a warm surgical incision site with delayed healing could be an early indication of infection. Another example is a hot, swollen area around an infected piercing, indicating a localized infection. The objective measurement of temperature, using tools like an infrared thermometer, provides concrete data for monitoring treatment response and documenting progress.
While assessing local warmth is a useful technique, it's crucial to consider its limitations. Normal inflammatory processes associated with wound healing also cause some degree of warmth, making it important to distinguish between normal and infection-related heat. It can be challenging to assess warmth accurately in cold environments, as the ambient temperature can affect skin temperature. Similarly, in areas with poor circulation, the temperature difference may be less noticeable.
To effectively assess local warmth as a sign of infection, use the back of your hand to gauge the temperature difference, as it is more sensitive than your palm. Compare the temperature of the wound area with an identical area on the opposite side of your body to provide a baseline. Check the temperature at the same time each day for consistency and to track any changes. Documenting changes in warmth intensity can be helpful in monitoring the infection's progression and response to treatment. Regularly monitoring wound temperature, combined with observation of other signs of infection, allows for early detection and timely intervention, which is crucial for effective wound management. This approach is especially important for patients with chronic wounds, like diabetic foot ulcers, where infections can have serious consequences. By staying vigilant and informed, patients and caregivers can play an active role in preventing and managing wound infections.
5. Swelling and Edema: A Key Indicator of Wound Infection
Swelling and edema are prominent signs of infected wound and warrant careful attention. This sign deserves its place on the list because it's often one of the earliest and most visible indicators of a developing infection. Understanding how to recognize and monitor swelling is crucial for both patients and healthcare professionals in managing wound healing effectively and preventing complications. Essentially, swelling around a wound signifies the body's natural inflammatory response trying to fight off harmful invaders. While a certain degree of swelling is expected after an injury as the body initiates the healing process, excessive or persistent swelling and edema often point towards a more serious issue – a potential infection.
So how does this work? When a wound becomes infected, bacteria and other pathogens invade the tissues. The body's immune system responds by sending white blood cells and other immune factors to the site of infection to combat these invaders. This influx of cells and fluids leads to an accumulation of fluid in the tissues surrounding the wound, causing visible swelling and edema.
Features of Infection-Related Swelling and Edema:
- Noticeable increase in tissue volume around the wound: The area around the wound will appear visibly larger than normal.
- Skin appears stretched or tight: The increased fluid volume stretches the skin, making it appear taut and shiny.
- Pitting may occur when pressed: Applying gentle pressure to the swollen area may leave a temporary indentation, known as pitting edema.
- Progressive worsening rather than improvement: Unlike normal post-injury swelling, infection-related edema tends to worsen over time instead of gradually subsiding.
- May affect wound closure or healing: Significant swelling can impede the wound's ability to close and heal properly.
Advantages of Monitoring Swelling and Edema:
- Visible sign that’s easy to monitor: Swelling is a readily observable sign, making it easy for patients and caregivers to track its progress.
- Can be measured objectively: The circumference of the swollen area can be measured with a tape measure, providing an objective assessment of the edema.
- Often correlates with other infection signs: Swelling frequently accompanies other signs of infection, such as redness, heat, pain, and purulent drainage.
Disadvantages of Relying Solely on Swelling and Edema:
- Can result from other causes like trauma or positioning: Swelling can also occur due to factors unrelated to infection, such as direct trauma to the area or prolonged immobility.
- May be normal in the immediate post-injury period: Some degree of swelling is expected immediately following an injury and doesn't necessarily indicate infection.
- Difficult to assess in already swollen areas: Evaluating changes in swelling can be challenging in areas that are already swollen due to pre-existing conditions.
Examples of Infection-Related Swelling:
- A swollen ankle surrounding an infected foot wound.
- A puffy eyelid resulting from an infected facial laceration.
- A swollen finger due to an infected hangnail.
Tips for Monitoring Swelling and Edema:
- Measure the circumference: Use a tape measure to measure the circumference of the swollen area at the same location each day.
- Compare with the unaffected limb: If possible, compare the swelling to the corresponding area on the opposite, unaffected limb.
- Note any impact on movement: Observe if the swelling restricts normal movement or range of motion.
- Document progression with photos: Taking regular photographs can help track the progression of the swelling over time.
Recognizing and monitoring swelling and edema is vital in managing wound care. While some swelling is a natural part of the healing process, persistent or increasing edema is a red flag that warrants further evaluation. By understanding the characteristics of infection-related swelling and utilizing the provided tips for monitoring, patients and healthcare providers can play a crucial role in identifying and addressing wound infections promptly. For those seeking further information on wound care and management, learn more about Swelling and Edema. Early intervention is key to preventing complications and promoting optimal healing. Always consult with a healthcare professional if you suspect a wound has become infected. This is crucial for individuals dealing with chronic wounds, as they are more susceptible to infections. For patients in long-term care facilities and communities, vigilant monitoring of wounds for signs of infection like swelling is particularly important due to their often-compromised immune systems. Primary care providers, wound care specialists, and other healthcare practitioners can use this information to better educate their patients, especially elderly patients and Medicare/insurance beneficiaries, on the signs of infected wounds and the importance of seeking timely medical attention.
6. Delayed or Impaired Healing: A Critical Sign of Infected Wound
Delayed or impaired healing is a significant indicator of a potentially infected wound and warrants careful attention. A wound that isn't healing as expected is a clear sign that something is amiss, often signaling an infection that's interfering with the natural healing process. This makes it a vital factor to consider when assessing wounds and a crucial inclusion in any list of signs of infected wound. Understanding the normal progression of wound healing is key to recognizing when a wound has stalled or veered off track.
Normal wound healing follows a predictable timeline and involves several overlapping phases: hemostasis (stopping bleeding), inflammation (cleaning the wound), proliferation (rebuilding tissue), and maturation (remodeling). Each phase plays a critical role, and disruptions, often caused by infection, can significantly hinder the entire process. Bacteria present in an infected wound can prolong the inflammatory phase, delay the formation of new tissue, and ultimately impede complete closure. This is why delayed healing deserves a prominent place on the list of signs of infected wound.
Features of Delayed or Impaired Healing:
Several characteristics can point towards delayed healing, all of which should be carefully monitored:
- Lack of healing progress after the expected timeframe: Different wound types have different healing timelines. A surgical incision should show significant progress within a few weeks, whereas a chronic ulcer might take considerably longer. A lack of progress within the anticipated timeframe for the specific wound type should raise concerns.
- Wound edges that fail to approximate: Healthy wounds gradually close as new tissue forms. If the wound edges remain separated or start to widen, it can indicate an underlying infection.
- No reduction in wound size over time: Similar to the previous point, a persistent wound size without any noticeable reduction can be a red flag.
- Development of new areas of breakdown: The appearance of new areas of skin breakdown or ulceration around the existing wound suggests the infection might be spreading.
- Poor tissue quality or unhealthy appearance: The wound bed might appear pale, dusky, or excessively granular. The surrounding skin might be discolored, swollen, or excessively tender.
Pros of Recognizing Delayed Healing:
- Indicates need for treatment modification: Recognizing delayed healing allows for timely adjustments to the treatment plan. This might involve debridement, topical or systemic antibiotics, or advanced wound care modalities.
- Can prevent progression to chronic wounds: Early intervention can significantly reduce the risk of a wound becoming chronic, which can be debilitating and challenging to manage.
- Useful for monitoring treatment effectiveness: Tracking healing progress helps assess the efficacy of the current treatment and make necessary changes if needed.
Cons of Relying on Delayed Healing as Sole Indicator:
- Requires knowledge of normal healing timelines: Accurately assessing delayed healing requires an understanding of typical healing times for different wound types and individual patient factors.
- Can be caused by factors other than infection: Conditions like diabetes, poor circulation, malnutrition, and certain medications can also impair wound healing, even in the absence of infection.
- May not be apparent in early stages: Subtle delays in healing might not be immediately obvious, particularly in chronic wounds.
Examples of Delayed Healing:
- A diabetic ulcer that remains the same size for weeks despite appropriate care.
- A surgical incision that reopens or widens, potentially accompanied by increased drainage or pain.
- A simple cut that doesn't close after 10-14 days.
Actionable Tips for Monitoring Wound Healing:
- Track wound dimensions weekly with a ruler or photography: Regular measurements provide objective data to monitor healing progress.
- Note changes in wound bed appearance: Document any changes in color, texture, or the amount of drainage.
- Monitor for new areas of skin breakdown: Pay close attention to the skin surrounding the wound for any signs of deterioration.
- Compare healing rate to healthcare provider's expectations: Discuss the expected healing timeline with your healthcare provider and report any deviations promptly.
Learn more about Delayed or Impaired Healing
By understanding the significance of delayed healing and vigilantly monitoring wound progress, patients and healthcare providers can work together to identify potential infections early, optimize treatment strategies, and promote effective healing. This attentive approach is crucial for preventing complications and improving outcomes in both acute and chronic wounds.
7. Systemic Symptoms (Fever, Malaise, Lymphadenopathy)
While many signs of a wound infection are localized, some infections progress beyond the immediate wound area and begin to affect the entire body. These are known as systemic symptoms, and their presence indicates a potentially serious situation requiring prompt medical attention. This is why monitoring for systemic symptoms is crucial in managing any wound, making it a vital inclusion in this list of signs of an infected wound. Systemic symptoms are often a sign that the infection is no longer contained and may be spreading through the bloodstream or lymphatic system.
Understanding Systemic Symptoms in Wound Infections
Systemic symptoms occur when the body’s immune system launches a widespread response to fight an infection that has spread beyond the initial wound site. This systemic response can manifest in various ways, including:
- Fever: A temperature above 100.4°F (38°C) is a common indicator of a systemic infection. The body raises its temperature to try to inhibit the growth and spread of infectious organisms.
- Malaise: This refers to a general feeling of illness, discomfort, or unease. It can be difficult to describe but often includes fatigue, weakness, and a sense of being unwell.
- Lymphadenopathy: This involves swelling of the lymph nodes, particularly those located near the infected wound. Lymph nodes are part of the body’s immune system and act as filters, trapping bacteria and other harmful substances. Swollen, tender lymph nodes indicate that the immune system is actively fighting an infection.
- Chills and Night Sweats: These are often associated with fever and can be a sign the body is struggling to regulate its temperature in response to infection.
- Loss of Appetite and Nausea: These digestive symptoms can also occur as the body diverts energy towards fighting the infection, potentially impacting normal metabolic processes.
Why Systemic Symptoms Warrant Attention
Systemic symptoms are a clear indication that a wound infection is becoming more serious and may require more aggressive treatment than topical antibiotics or simple wound care. Ignoring these signs can lead to severe complications, including sepsis (a life-threatening condition caused by the body’s overwhelming response to infection) or even organ damage. Therefore, if you experience any systemic symptoms alongside a wound, it's crucial to seek medical advice immediately.
Pros and Cons of Using Systemic Symptoms as an Indicator:
Pros:
- Indicates Severity: The presence of systemic symptoms clearly signals the need for prompt and potentially aggressive medical intervention.
- Objective Measurement: Fever, a key systemic symptom, can be objectively measured with a thermometer, providing concrete evidence of infection.
- Distinguishes Local from Systemic Infection: Systemic symptoms help differentiate a localized wound infection from one that has spread throughout the body.
Cons:
- May Indicate Advanced Infection: The appearance of systemic symptoms often suggests the infection has already progressed and may require hospitalization.
- Can be Caused by Other Illnesses: Systemic symptoms are not exclusive to wound infections and can be present in other conditions, requiring careful diagnosis.
- Blunted in Immunocompromised Patients: Individuals with weakened immune systems may not exhibit the typical systemic symptoms, even with a serious infection, making diagnosis more challenging.
Examples of Systemic Symptoms in Wound Infections:
- A patient with an infected surgical wound develops a fever and chills.
- An individual with an infected hand cut experiences swollen and tender lymph nodes in their armpit.
- A person with an infected leg ulcer suffers from fatigue and loss of appetite.
Actionable Tips for Monitoring and Managing Systemic Symptoms:
- Monitor Temperature: Take your temperature twice daily with an accurate thermometer, especially if you have a wound.
- Check Lymph Nodes: Regularly examine the lymph nodes in the areas draining the wound for any swelling or tenderness.
- Note Changes in Energy Level and Appetite: Pay attention to any unusual fatigue, weakness, loss of appetite, or nausea.
- Keep a Log: Maintain a detailed record of any systemic symptoms you experience, including their onset, duration, and severity. This information will be helpful for your healthcare provider.
Learn more about Systemic Symptoms (Fever, Malaise, Lymphadenopathy)
If you observe any systemic symptoms associated with a wound, it is essential to contact a healthcare professional immediately. Early diagnosis and treatment are critical for preventing serious complications and ensuring a successful recovery. This proactive approach to wound management can significantly impact patient outcomes, especially in vulnerable populations like the elderly or those with chronic conditions. For healthcare providers, recognizing and addressing systemic symptoms related to wound infections is crucial for providing comprehensive and effective care.
7 Key Signs of Wound Infection Comparison
| Sign or Symptom | 🔄 Implementation Complexity | 💡 Resource Requirements | 📊 Expected Outcomes | ⚡ Ideal Use Cases | ⭐ Key Advantages |
|---|---|---|---|---|---|
| Increased Pain or Tenderness | Low – Patient self-monitoring | Minimal – Pain diary, observation | Early detection before visual changes | Early infection warning, post-surgical wounds | Easily monitored, prompts early intervention |
| Purulent Discharge (Pus Formation) | Moderate – Visual assessment, culture possible | Moderate – Clean gauze, lab access | Highly specific bacterial infection indicator | Wounds with visible drainage, suspected infection | Easily recognizable, culturable for diagnosis |
| Erythema (Redness) Spreading Beyond Wound Edges | Moderate – Regular measurement and marking | Low – Pen, ruler for tracking | Indicates spreading infection, guides antibiotic use | Monitoring expanding wound inflammation | Visible early sign, measurable progression |
| Local Warmth and Heat | Low to Moderate – Touch or thermometer | Minimal to Moderate – Infrared thermometer optional | Early inflammation sign, treatment monitoring | Detecting infection before visual signs | Objective measurement option, early detection |
| Swelling and Edema | Moderate – Measurement and observation | Minimal – Measuring tape, photo documentation | Indicates fluid accumulation and worsening infection | Monitoring wound area changes | Easy visual monitoring, correlates with other signs |
| Delayed or Impaired Healing | Moderate – Regular wound assessment | Minimal – Ruler, photography | Detects failure of healing, signals treatment review | Chronic wounds, slow-healing injuries | Prevents chronic wound progression |
| Systemic Symptoms (Fever, Malaise, Lymphadenopathy) | Moderate – Monitoring vitals and symptoms | Moderate – Thermometer, clinical evaluation | Indicates severe or spreading infection | Systemic infection detection, severe cases | Objectively measurable, signals urgent care |
Taking Action: Next Steps for Wound Care
Recognizing the signs of an infected wound is crucial for effective treatment and preventing complications. This article has outlined seven key indicators to watch for: increased pain, pus formation, spreading redness, localized heat, swelling, slow healing, and systemic symptoms like fever. Mastering these concepts empowers you to take proactive steps in managing your wound care, potentially minimizing discomfort and promoting faster recovery. Early detection and intervention are key to preventing serious health issues that can arise from untreated infected wounds.
If you observe any of these signs of infected wound, don't hesitate to seek professional medical advice. Prompt treatment is essential to prevent the infection from spreading and causing further complications. Proper wound care can significantly improve healing outcomes and your overall well-being.
Don't let a potential infection compromise your health. Rapid Wound Care specializes in the effective treatment of infected wounds and other complex wound conditions. Visit Rapid Wound Care today to learn more about our comprehensive services and how we can help you on your path to healing.

