A debridement procedure is a medical process where a clinician carefully removes dead, damaged, or infected tissue from a wound. This is a critical first step for any wound that has stalled and isn't healing on its own, essentially clearing the way for healthy new tissue to grow.
Why Debridement Is a Critical Reset for Healing

Think of a garden plot that’s completely overrun with weeds and dead plants. You can water it and add all the fertilizer you want, but nothing new will grow until you clear out all that debris. A non-healing wound is a lot like that garden, where dead tissue (we call it necrotic tissue) acts like weeds, physically blocking healthy cells from regenerating.
A debridement procedure is the clinical version of weeding that garden. It isn't just a simple cleaning—it's a precise medical intervention meant to "reset" the wound's environment. By strategically removing the unhealthy tissue, we eliminate the barriers that are holding back the body's natural healing capabilities.
The Core Goals of Debridement
This procedure is a true cornerstone of modern wound care, especially for chronic issues like pressure sores, severe burns, and other complex injuries. It's also absolutely essential for managing serious conditions like diabetic foot ulcers, where poor circulation often gets in the way of natural healing. For a deeper dive, check out our guide on treating diabetic foot ulcers.
The primary goals of any debridement are straightforward but powerful:
- Get rid of infection sources by removing tissue where bacteria thrive.
- Remove physical roadblocks that prevent new, healthy skin from forming.
- Stimulate the wound bed to jolt the healing process back into action.
By preparing the wound bed, debridement ensures that all subsequent treatments—from advanced dressings to specialized therapies—have the best possible chance of success. It creates a clean slate for healing to begin.
This essential first step is what makes further healing possible. Without it, even the most advanced treatments are likely to fail because the very foundation for recovery is compromised.
The table below breaks down the key reasons a clinician would perform this vital procedure.
Key Reasons for Performing a Debridement Procedure
This table summarizes the primary objectives and benefits of undergoing a debridement procedure for effective wound management.
| Objective | Explanation | Impact on Healing |
|---|---|---|
| Infection Control | Removes tissue colonized with bacteria, reducing the risk of local or systemic infection (sepsis). | Creates a cleaner wound environment and allows the body's immune system to work more effectively. |
| Barrier Removal | Clears away necrotic tissue (slough, eschar) that physically obstructs new cell growth. | Exposes healthy, bleeding tissue, which is necessary for the healing process to advance. |
| Healing Stimulation | The process itself can trigger the release of growth factors and improve blood flow to the area. | Actively encourages the wound to move from a chronic, stalled state to an active healing phase. |
Ultimately, debridement isn't just about removing the bad stuff; it's about making way for the good stuff. It’s a proactive step that shifts a wound from being stuck to actively healing.
Exploring the Different Types of Debridement
When it comes to wound care, choosing a debridement method isn't a one-size-fits-all situation. Think of a wound care specialist's toolkit—it’s filled with different instruments and techniques, each designed for a specific job. The right choice hinges on the wound itself, the patient's overall health, and the ultimate healing goal.
You wouldn't use a sledgehammer for a delicate sculpture, and you wouldn't use a tiny chisel to break up a concrete slab. It’s the same with debridement. The method has to match the challenge presented by the wound.
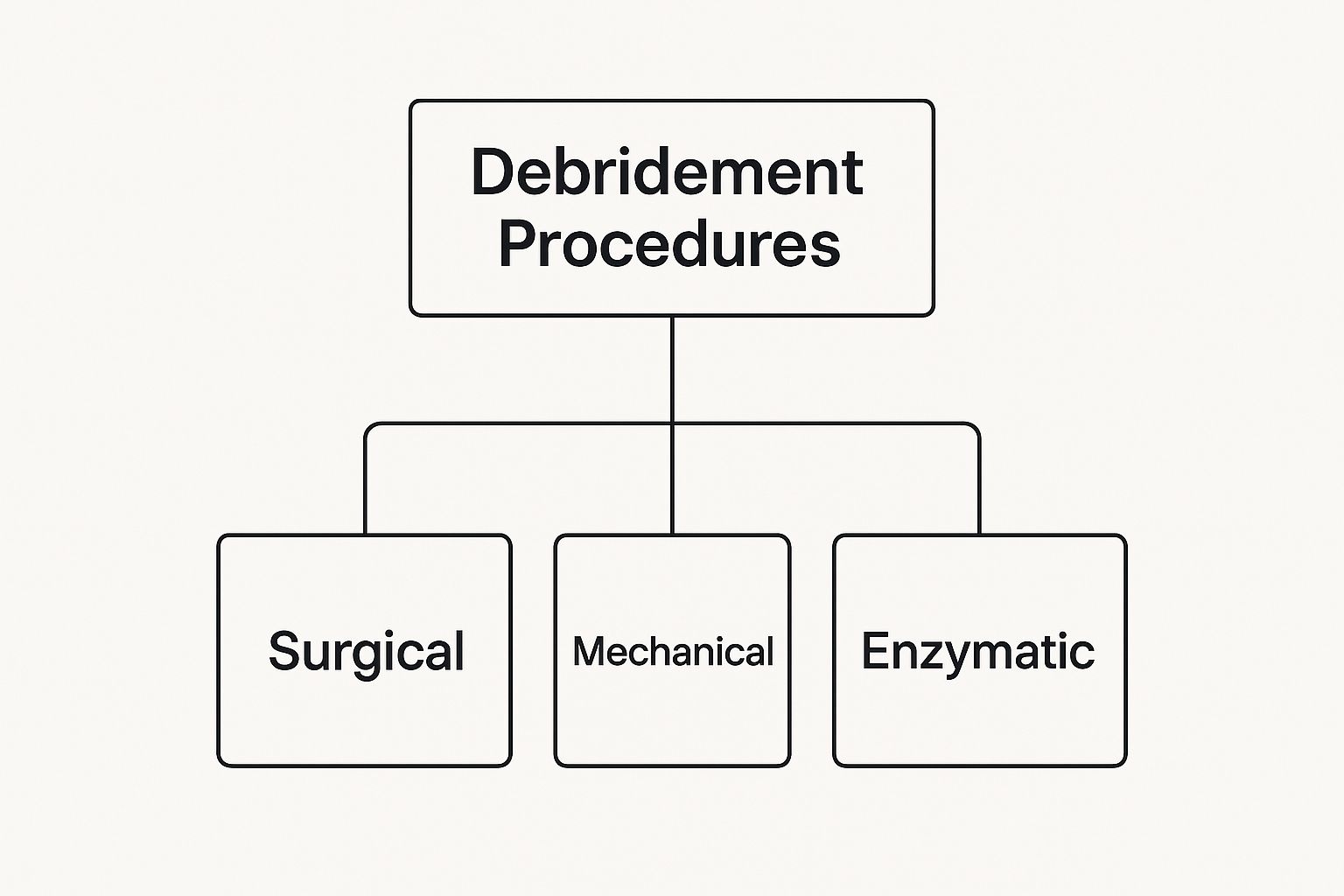
As you can see, debridement isn't just one thing. It branches out into several distinct approaches for cleaning the wound bed. Let's break down what these are and when a clinician would choose one over the other.
H3: Surgical Debridement: The Sculptor’s Precision
Surgical debridement is the most direct and aggressive method, performed by a surgeon or podiatrist with sharp instruments like scalpels and scissors. This is usually done in a sterile setting, like an operating room.
Imagine a sculptor carefully chipping away flawed stone to reveal a perfect statue. That's the kind of precision we're talking about. The clinician meticulously removes dead or infected tissue, layer by layer, preserving every bit of healthy tissue underneath. It’s fast, thorough, and often the best choice for large wounds, deep infections, or when time is of the essence.
H3: Mechanical Debridement: A Less Selective Approach
Unlike the surgical approach, mechanical debridement physically removes dead tissue without precise cutting. This category covers techniques like hydrotherapy (using water to wash away debris) or wet-to-dry dressings, where a moist gauze dries and sticks to dead tissue, pulling it away when changed.
Think of this method less like a sculptor and more like pressure washing a dirty surface. It's effective for clearing away loose debris, but it’s non-selective. That means it can sometimes take healthy, new tissue along with the bad. For this reason, it's used more cautiously today but still has its place.
H3: Enzymatic Debridement: The Biological Dissolver
Enzymatic debridement uses a special kind of medicine—a prescribed ointment or gel packed with enzymes. These enzymes are like biological dissolvers, specifically targeting and breaking down dead tissue while leaving healthy cells completely alone.
This approach is incredibly selective and painless, which makes it a great option for patients who can't undergo surgery. It’s a slower process that requires daily applications, but its precision is a huge benefit, especially in treating burns where it's critical to tell damaged tissue from healthy. If you're dealing with more complex injuries, our guide on the 6 types of wounds can offer some extra context.
H3: Autolytic Debridement: The Body’s Own Crew
Autolytic debridement is the gentlest method of all. It actually uses the body’s own healing mechanisms, boosted by modern dressings that create a moist wound environment. Dressings like hydrocolloids or hydrogels trap the body’s natural enzymes at the wound, letting them work their magic to liquefy and separate the dead tissue.
Think of it as creating the perfect "greenhouse" for your body's clean-up crew to get the job done right. It’s a very slow but highly selective process, making it ideal for smaller, non-infected wounds.
H3: Biosurgical Debridement: Nature’s Microsurgeons
Finally, we have biosurgical debridement, which is sometimes called maggot therapy. Yes, you read that right. This method uses sterile, medical-grade larvae to clean a wound. These tiny creatures secrete enzymes that dissolve only dead tissue and bacteria, leaving healthy tissue completely untouched.
It might sound a little strange, but it’s an incredibly effective and FDA-approved technique for stubborn, non-healing wounds. In essence, it harnesses nature’s own microsurgeons to perform a highly precise cleaning job.
When Is a Debridement Procedure Necessary?
A debridement procedure isn't just a simple cleaning. It's a targeted medical intervention for wounds that have hit a wall and can't heal on their own. This happens when the body's natural healing process gets overwhelmed, and dead tissue starts to build up, acting as a major roadblock to recovery.
Think of it like trying to build a new house on a foundation cluttered with debris. You can't lay down new materials until you clear the old junk away. A wound works the same way. When it's covered in necrotic tissue (dead tissue), new, healthy cells can't form. Worse, that dead tissue becomes a perfect breeding ground for harmful bacteria.
This is where a clinician steps in. They assess the wound to see if it has stalled, and if debridement is the key to restarting the healing engine.
Common Scenarios Requiring Debridement
Some medical conditions are notorious for creating non-viable tissue, making debridement a necessary step. Each one presents its own set of challenges that stop the body from repairing itself.
- Diabetic Foot Ulcers: In people with diabetes, poor circulation and nerve damage (neuropathy) are a dangerous combination. A small cut can go unfelt and, starved of oxygen-rich blood, the tissue dies. This creates an ulcer that’s extremely vulnerable to infection.
- Pressure Injuries (Bedsores): These wounds form when constant pressure, usually over bony spots like the hips or tailbone, chokes off blood flow. Without blood, the skin and underlying tissue break down, leading to a chronic wound that only gets deeper if the dead layers aren't removed.
- Severe Burns: Burns instantly kill skin cells, creating a tough, leathery layer of dead tissue called eschar. This eschar acts like a tight, restrictive cap. Debridement is vital not just to head off infection but also to release pressure and give the healthy tissue underneath a chance to survive.
- Traumatic Injuries: A deep gash, crush injury, or any wound contaminated with foreign debris like dirt or gravel will almost always contain damaged tissue. Clearing it out is the first critical move to prevent a massive infection and set the stage for proper healing. In fact, learning how to heal deep wounds faster often starts with a thorough debridement.
The Clinician's Assessment Process
The decision to debride a wound is never taken lightly. A healthcare provider conducts a careful, detailed assessment, looking at several key factors to get the full picture.
First, they check the type of tissue in the wound bed. Healthy tissue looks pink or red and has good blood flow. Unhealthy tissue, however, might be yellow (slough) or black (eschar)—both are clear signals that debridement is on the table.
A wound cannot progress from the inflammatory phase to the proliferative (rebuilding) phase of healing as long as necrotic tissue is present. Its removal is the trigger that signals the body it's time to start rebuilding.
Next, the provider hunts for signs of infection. This could be increased redness, swelling, warmth, a foul smell, or pus. Removing infected tissue is absolutely critical to prevent the infection from escaping into the bloodstream and causing sepsis, which is life-threatening.
Finally, they gauge the wound's depth. The procedure must be thorough enough to remove all compromised layers, whether it's just skin, or goes down into fat, fascia, muscle, or even bone. According to official coding guidelines, the procedure is defined by the deepest layer of tissue removed. So, if debridement reaches muscle, the entire procedure is coded as a muscle debridement.
This complete evaluation ensures debridement is only used when absolutely necessary—as the key action that shifts a wound from a chronic, stalled state onto the path toward full recovery.
What to Expect During the Debridement Procedure
Thinking about any medical procedure can be a little nerve-wracking, but knowing exactly what's coming can make a world of difference. A debridement procedure isn't as scary as it might sound; it’s a highly controlled and meticulous process designed to clear the way for your body to heal.
Let's walk through what actually happens—from getting ready for the procedure to the immediate aftercare. Understanding these steps can help you feel more confident and in control of your healing journey. The whole thing can be broken down into three simple phases: preparation, the procedure itself, and what happens right after.
The Preparation Phase
Before a single instrument is picked up, your healthcare team does some important homework. This first step is all about careful planning to make sure the procedure is as safe and effective as possible for you.
A clinician will take a close look at your wound, noting its size, depth, and what kind of unhealthy tissue is present. They'll also review your overall health history to tailor the debridement method specifically to your needs.
Pain management is a huge priority here. Based on the wound and the type of debridement planned, your doctor will choose the right anesthetic to keep you comfortable.
- Local Anesthesia: For smaller wounds or procedures done right at your bedside, this is the go-to option. It involves an injection that completely numbs the wound and the area around it. You'll be awake, but you won't feel any pain during the debridement.
- General Anesthesia: For more serious surgical debridement, especially for deep wounds or large areas, you'll likely be in an operating room under general anesthesia. This means you’ll be completely asleep and pain-free for the entire process.
No matter which option is chosen, the team won't start until you are comfortable and properly medicated.
Inside the Procedure Room
Once the area is numb or you're asleep, the debridement procedure can begin. This is where the skill of the surgeon or specialist really comes into play. The environment is kept completely sterile—think gowns, gloves, and masks—to prevent any new bacteria from getting into the wound.
Using precise tools like scalpels, curettes, or special scissors, the clinician carefully removes the dead or infected tissue. It's almost like a sculptor meticulously chipping away unwanted material to reveal the healthy, viable foundation underneath. They work with extreme precision to protect the healthy, bleeding tissue, as this is the raw material your body will use to build new skin. The goal is to be aggressive enough to remove all the bad stuff while preserving every bit of healthy tissue possible.
The concept of meticulously cleaning a wound to promote healing isn't new. This idea laid the foundation for modern wound care practices, proving that a clean wound bed is the first step toward recovery.
This methodical approach has a surprisingly long and proven history. The powerful combination of physical cleaning and antiseptic methods was first formally studied by military surgeon Carl von Reyher during the Russo-Turkish wars in the late 1870s. His work resulted in a stunning 43% reduction in mortality among his patients, proving just how critical a thorough debridement is. You can read more about the evolution of debridement on ezdebride.com.
Immediate Post-Procedure Care
As soon as the debridement is finished, the final stage begins. The first thing your clinician will do is gently clean the newly exposed wound bed, usually with a saline solution, to wash away any lingering debris.
Next comes a fresh, clean dressing. The type of dressing isn't one-size-fits-all; it’s chosen based on your wound's specific needs. It might be a simple gauze or a more advanced dressing made to manage moisture and provide extra protection. Think of this dressing as the wound's first line of defense as the healing process kicks into high gear.
Your clinical team will then watch you for a little while to check for any immediate issues, like too much bleeding. Before you head home or back to your room, you’ll get your first set of recovery instructions—how to care for the dressing, what signs of infection to look out for, and how to manage any discomfort. This clear plan takes the mystery out of the experience, showing it for what it is: a controlled, purposeful step on your path to healing.
Navigating Recovery and Post-Procedure Care

A successful debridement procedure is just the first step. The real work—the healing—begins in the days and weeks that follow. Think of it like this: the procedure cleared the construction site, but now your body needs the right materials and a solid blueprint to start rebuilding. That blueprint is your aftercare.
Your recovery journey is a partnership between you and your provider. Sticking to their instructions is non-negotiable. This care is specifically designed to protect the fresh, healthy tissue that was just uncovered and give it the absolute best environment to thrive.
Your Role in At-Home Wound Management
Once you’re home, you become the primary guardian of your healing wound. Your provider will give you specific directions, but your responsibilities will boil down to three key things: managing pain, keeping the wound clean, and watching for any signs of trouble.
It’s normal to feel some discomfort as the anesthesia wears off. Your provider will lay out a pain management strategy, which often involves over-the-counter options like ibuprofen or acetaminophen. The trick is to stay ahead of the pain. This helps you rest comfortably and move around as advised, which is great for circulation and healing.
Proper wound care, however, is probably your most critical task. This usually involves:
- Dressing Changes: You'll get a schedule for changing your dressing. Follow it to the letter. This is essential for keeping the wound clean and maintaining the right moisture balance.
- Cleaning the Wound: You’ll likely be told to gently clean the area with a specific solution, most often saline. Steer clear of harsh chemicals like hydrogen peroxide unless your provider explicitly tells you to use them—they can damage the delicate new cells your body is working so hard to create.
- Hand Hygiene: This is a big one. Always wash your hands thoroughly with soap and water before and after touching your wound or its dressing. This simple step is your best defense against introducing new bacteria.
For a deeper dive, learning about effective post-discharge wound care at home can give you extra confidence and clarity as you heal.
Recognizing and Responding to Complications
While most people recover without a hitch, it’s vital to know what to look for. Catching a problem early is the secret to getting it under control quickly.
A vigilant eye is your best defense. Noticing a small change early on can prevent a minor issue from turning into a major setback for your recovery.
Get in touch with your healthcare provider immediately if you spot any of these red flags:
- Increasing Pain: Pain that gets suddenly worse or doesn't improve with your prescribed medication.
- Signs of Infection: This can include growing redness, swelling, warmth spreading from the wound, a foul smell, or thick, discolored drainage (pus).
- Fever: A temperature of 101°F (38.3°C) or higher could signal a systemic infection.
- Excessive Bleeding: A little spotting on the dressing can be normal, but any bleeding that soaks through is a cause for concern.
Fueling Your Body for Healing
Never underestimate the power of good nutrition. Your body is working overtime to build new tissue, and that process demands extra energy and specific nutrients. Zero in on a balanced diet that’s rich in protein—it provides the essential building blocks for new skin and blood vessels.
Hydration is equally important. Staying well-hydrated helps shuttle all those good nutrients to the wound site and keeps your skin healthy and pliable. Make it a goal to drink plenty of water all day long. By managing your wound carefully and fueling your body properly, you set the stage for a smooth, successful recovery.
Innovations and Modern Applications in Debridement
While the core principles of a debridement procedure are timeless, its applications are anything but static. This fundamental practice is constantly evolving and has become a critical component in a whole host of specialized surgeries. It's no longer just about cleaning up a stubborn chronic wound; it’s about giving surgeons the tools to optimize outcomes in complex orthopedic and reconstructive procedures.
Take carpal tunnel release surgery, for instance. Debridement here isn't about removing dead skin. Instead, the surgeon meticulously clears away the inflamed synovial tissue that's squeezing the median nerve. This precise removal of problematic tissue is exactly what alleviates the debilitating pain and numbness of the condition, proving just how targeted debridement has become.
New Techniques and Evolving Trends
The field is also seeing a major push toward less invasive techniques that make a real difference in patient recovery. We see this clearly in hand surgery, where the data shows a distinct shift away from traditional open surgery toward minimally invasive endoscopic methods for certain conditions.
For example, carpal tunnel release (CTR), which often incorporates debridement, has an incidence rate of 32.2 per 100,000 people over age 20. Interestingly, an analysis from fessh.com reveals that regions with more hand surgery specialists tend to have a higher rate of endoscopic CTR. This points to a strong link between specialized training and the adoption of modern, less invasive approaches.
This evolution directly benefits the patient. Minimally invasive methods mean smaller incisions, less pain after surgery, and a much shorter recovery time. Patients can get back to their lives and regain function far more quickly.
The evolution of the debridement procedure highlights a key goal in modern medicine: achieving the best possible clinical outcome with the least amount of physical impact on the patient. It's about working smarter, not just harder.
The Bigger Picture in Surgical Care
These advancements also show how debridement fits into a more holistic approach to surgical care. Think about an ankle ligament reconstruction. Before repairing the ligaments, a surgeon might perform an arthroscopic debridement to "clean up" the joint, removing scar tissue and bone spurs that are causing irritation.
This initial clean-up is crucial. By getting rid of these mechanical irritants, the surgeon creates a healthier environment within the joint, which can lead to less long-term pain and better stability after the repair.
Whether it's performed in a hospital or as part of a broader treatment plan, the goal is always the same. In fact, understanding how home wound care speeds up recovery after these procedures is a key piece of the healing puzzle. From orthopedic repairs to advanced wound management, debridement remains an essential tool, continually adapting to meet new challenges.
Answering Your Questions About Debridement
Even after getting the basics down, it’s completely normal to have questions about what the experience is really like. Getting clear, honest answers can do wonders for your peace of mind and help you feel ready for the healing journey ahead. Let's tackle some of the most common concerns we hear from patients.
Is the Debridement Procedure Painful?
Pain management is always a top priority, and we make sure you’re comfortable from start to finish. For smaller debridements done in a clinic, your provider will use a local anesthetic to completely numb the wound and the skin around it. You might feel some pressure during the work, but you shouldn't feel pain.
If you have a larger wound that requires surgical debridement in an operating room, you'll likely be given regional or general anesthesia. This ensures you're completely pain-free and comfortable throughout. It’s normal to feel some soreness afterward, but your doctor will set you up with a solid pain management plan to keep you comfortable during recovery.
How Long Does Recovery Take?
This is one of the most common questions, but the answer is always: it depends. Recovery time varies quite a bit based on a few key factors: the size and depth of your wound, the type of debridement performed, and your overall health.
A minor procedure might only take a few weeks to heal up. On the other hand, a more significant debridement for a chronic wound could take several months. Your healthcare provider is your best guide here—they’ll give you a personalized timeline and schedule follow-ups to make sure everything is healing as it should.
The most important part of recovery is patience. Healing is not always a linear process, and giving your body the time it needs is crucial for a successful outcome.
Will I Have a Scar After the Procedure?
Scarring is a natural part of how our bodies heal whenever the skin is broken, so yes, some level of scarring is unavoidable. The final look of a scar really depends on the wound’s depth and location, your own genetics, and how well you follow your aftercare instructions.
But here's the upside: the whole point of debridement is to create a clean, healthy foundation for the wound to heal properly. This almost always leads to a much better cosmetic result than if that unhealthy tissue was left behind. Once your wound is fully closed, you can chat with your doctor about scar management options to minimize its appearance.
Can Debridement Be Done More Than Once?
Yes, absolutely. In fact, it's quite common for patients managing complex or chronic wounds, like diabetic ulcers or severe pressure injuries, to need more than one debridement over time.
Think of it this way: healing is a dynamic journey. Sometimes, unhealthy tissue can reappear, especially if the underlying problem causing the wound hasn't been fully resolved. Repeated procedures are often a key part of the long-term strategy to keep the wound bed clean and keep pushing it toward that final closure. Each debridement acts as a "reset," giving the wound another strong chance to heal.
At Rapid Wound Care, we understand that healing happens at home. Our certified professionals bring advanced wound care, including expert debridement and personalized treatment plans, directly to you, minimizing stress and maximizing comfort. If you or a loved one needs dedicated support for a complex wound, let our team help you get on the path to recovery. Learn more about our at-home services.

