A Comprehensive Guide to Effective Wound Care
Proper wound care best practices are essential for healing and preventing complications. This guide provides eight key practices to optimize wound care, whether you're managing a minor injury or a chronic condition. Learn how to perform a thorough wound assessment, maintain moisture balance, prevent infections, and manage tissue effectively. We'll also cover pressure redistribution, nutritional support, patient education, and the importance of a multidisciplinary approach. Following these wound care best practices can significantly improve healing outcomes and overall well-being.
1. Comprehensive Wound Assessment
Effective wound care hinges on accurate and thorough assessment. A comprehensive wound assessment is the cornerstone of best practices, providing the foundation for developing an effective treatment plan and monitoring progress. It's a systematic evaluation of both the wound itself and the patient's overall health, identifying factors that might influence healing. This crucial first step guides all subsequent decisions, ensuring the best possible outcome for patients experiencing both acute and chronic wounds. By meticulously documenting wound characteristics, understanding the underlying causes, and considering individual patient factors, healthcare professionals can establish realistic healing goals and optimize treatment strategies.

This approach goes beyond simply looking at the wound. It involves a multi-faceted evaluation encompassing several key areas: precise documentation of the wound's size, depth, location, and visual appearance (including tissue type and exudate characteristics); assessment of the periwound skin; a thorough patient history, including any comorbidities that might impact healing (such as diabetes, vascular disease, or malnutrition); a vascular assessment to determine blood flow to the affected area; and infection screening. This detailed information paints a complete picture of the wound and the individual's overall health status, enabling a personalized and targeted treatment plan.
The benefits of a comprehensive wound assessment are numerous. It facilitates evidence-based treatment planning, allowing healthcare providers to select the most appropriate interventions based on the specific characteristics of the wound and patient needs. It establishes a crucial baseline for monitoring healing progress and helps identify potential barriers to healing, like infection or inadequate blood supply. This proactive approach can prevent complications and promote faster, more efficient recovery. Furthermore, a comprehensive assessment promotes effective communication between healthcare providers, ensuring everyone involved in the patient's care is working from the same information.
Real-world examples highlight the positive impact of structured wound assessments. The Cleveland Clinic, for example, implemented a standardized wound assessment protocol, resulting in a remarkable 23% reduction in healing time. The Mayo Clinic's adoption of a digital wound assessment system significantly improved documentation accuracy and streamlined the assessment process. Similarly, the Veterans Affairs implementation of a structured assessment program led to a demonstrable decrease in amputation rates. These examples underscore the value of incorporating comprehensive wound assessment into routine practice.
While the benefits are significant, there are also some challenges. A comprehensive wound assessment can be time-intensive, requiring skilled practitioners with specialized training. It may necessitate the use of multiple assessment tools and measurements, potentially increasing complexity. Furthermore, certain aspects of the assessment, such as pain evaluation, can be subjective, leading to variations between assessors. However, the advantages far outweigh the drawbacks, making it a crucial component of optimal wound care.
To maximize the effectiveness of wound assessment, consider these practical tips: utilize standardized assessment forms and validated measurement tools to ensure consistency and accuracy; incorporate photography for visual documentation and tracking of healing progress; reassess wounds at regular intervals to monitor changes and adjust treatment as needed; and always include a thorough patient pain assessment as part of the comprehensive evaluation, addressing both the physical and emotional impact of the wound.
This comprehensive approach to wound assessment has been widely popularized and championed by leading organizations in wound care, including the Wound Ostomy and Continence Nurses Society (WOCN) and the Association for the Advancement of Wound Care (AAWC). Prominent figures in the field, such as Dr. Caroline Fife, a renowned wound care pioneer, have also significantly contributed to its widespread adoption, advocating for its essential role in optimizing patient outcomes. By incorporating a comprehensive wound assessment into wound care best practices, patients and healthcare providers can work together to achieve successful healing and improved quality of life. This detailed initial evaluation provides the roadmap for effective treatment, ultimately minimizing complications and promoting optimal recovery.
2. Moisture Balance Management
Moisture balance management is a cornerstone of modern wound care best practices. It focuses on maintaining the optimal level of moisture within the wound bed to promote efficient healing while simultaneously preventing damage to the surrounding healthy tissue. This delicate balance is achieved through careful selection of appropriate dressings and diligent management of exudate—the fluid that seeps from a wound. By creating this ideal healing environment, moisture balance management significantly improves patient outcomes and reduces healing time.

The principle behind moisture balance management is simple yet powerful. A dry wound bed impedes cellular migration and delays the healing process. Conversely, excessive moisture can macerate, or soften and damage, the surrounding skin, increasing the risk of infection. Therefore, the goal is to maintain a "Goldilocks" level of moisture—not too wet, not too dry, but just right. This involves choosing dressings that either retain moisture in dry wounds or absorb excess moisture in heavily exuding wounds. Effective moisture balance management also includes protecting the periwound skin, the delicate tissue surrounding the wound itself, from the damaging effects of excessive moisture. This often involves using barrier creams or films.
The benefits of moisture balance management are well-documented. Studies have shown that maintaining optimal wound bed hydration accelerates cellular migration and tissue repair. This, in turn, leads to faster healing times. For example, Johns Hopkins Hospital implemented a moisture management protocol that reduced diabetic ulcer healing time by an impressive 30%. Furthermore, moisture-retentive dressings minimize pain and trauma during dressing changes, a significant advantage for patients, particularly those with chronic wounds. By keeping the wound bed moist, these dressings prevent the wound from sticking to the dressing, reducing discomfort and further tissue damage during removal. Another key advantage is the preservation of growth factors within the wound fluid. These growth factors are essential for tissue regeneration and are more concentrated in a moist environment.
The UK's National Health Service (NHS) provides further evidence of the effectiveness and cost-effectiveness of moisture balance management. Their implementation of moisture-retentive dressings has resulted in annual savings of £2.3 million. Similarly, wound care centers utilizing hydrocolloid dressings, a type of moisture-retentive dressing, have reported healing rates as high as 85%. These successes highlight the significant positive impact of this wound care best practice.
While the advantages of moisture balance management are numerous, it’s important to be aware of the potential drawbacks. This approach requires frequent monitoring and adjustment of the dressing regimen to ensure the optimal moisture level is maintained. Over-hydration can lead to maceration and increase the risk of infection, so careful assessment is vital. Additionally, some advanced moisture-balancing dressings can be more costly than traditional gauze dressings. However, the long-term benefits of faster healing and reduced complications often outweigh the initial expense.
To implement moisture balance management effectively, consider the following tips: Carefully match the absorption capacity of the dressing to the level of wound exudate. For heavily draining wounds, use highly absorbent dressings. For dry wounds, opt for moisture-retentive dressings like hydrogels. Always use barrier creams or films to protect the periwound skin from maceration. Monitor the wound daily for signs of either maceration (excessive moisture) or desiccation (drying out), and adjust the dressing type and frequency as needed. Learn more about Moisture Balance Management You might find resources helpful, such as those exploring wet-to-dry dressing changes and their role in wound care.
Pioneering work by Dr. George Winter, who championed the concept of moist wound healing, laid the foundation for modern moisture balance management. Innovations in wound dressing technology by companies like Smith & Nephew and 3M Healthcare have further advanced the practice, providing clinicians with a wide range of dressing options to address various wound types and exudate levels. Moisture balance management is a critical component of wound care best practices, offering a significant improvement over traditional dry wound management techniques. Its widespread adoption demonstrates its efficacy in promoting faster healing, reducing complications, and improving patient comfort.
3. Infection Prevention and Control
Infection prevention and control is arguably the most crucial aspect of wound care best practices. It encompasses a comprehensive approach to minimizing the risk of wound infections, a complication that can significantly impede healing, escalate healthcare costs, and even threaten a patient's life. By diligently adhering to proper hygiene, employing sterile techniques, practicing antimicrobial stewardship, and promptly recognizing the signs of infection, healthcare providers and patients can dramatically improve healing outcomes and overall quality of life. This element of wound care is so vital that it deserves a prominent place in any best practices list, as preventing infection is often easier, less expensive, and significantly less painful than treating one.
Wound infections occur when harmful microorganisms, such as bacteria, fungi, or viruses, invade the wound bed. These microbes can delay the healing process by interfering with tissue regeneration, prolonging inflammation, and causing further tissue damage. In severe cases, untreated wound infections can lead to sepsis, a life-threatening condition characterized by a systemic inflammatory response.
Why is Infection Prevention and Control Crucial in Wound Care?
Infection prevention and control plays a pivotal role in wound care for several key reasons:
- Improved Healing Outcomes: A clean, uninfected wound heals significantly faster and more efficiently. By preventing infection, we create the optimal environment for the body's natural healing processes to take place.
- Reduced Complications: Infections can lead to a cascade of complications, including abscess formation, cellulitis, osteomyelitis (bone infection), and sepsis. These complications can prolong recovery time, increase healthcare costs, and even be life-threatening.
- Enhanced Patient Comfort: Infected wounds are often painful, swollen, and produce foul-smelling drainage. Preventing infection minimizes patient discomfort and improves their overall well-being.
- Cost-Effectiveness: Preventing infection is significantly less expensive than treating an established infection. The costs associated with treating an infected wound can include prolonged hospital stays, additional medications, and specialized wound care procedures.
Key Features of Effective Infection Prevention and Control:
- Strict Hand Hygiene: Handwashing with soap and water or using an alcohol-based hand sanitizer before and after every wound contact is paramount. This simple act is one of the most effective ways to prevent the spread of infection.
- Sterile Technique: All wound care procedures, including dressing changes and wound debridement, should be performed using sterile technique to minimize the introduction of microorganisms into the wound bed.
- Regular Monitoring: Frequent assessment of the wound for signs and symptoms of infection is crucial. This includes monitoring for increased pain, redness (erythema), warmth, swelling, and the presence of purulent (pus-filled) drainage.
- Judicious Use of Antimicrobials: Antimicrobial dressings and systemic antibiotics should be used judiciously and only when clinically indicated. Overuse of antimicrobials can contribute to the development of antibiotic resistance, making future infections more difficult to treat.
- Isolation Precautions: In cases of highly contagious wound infections, implementing appropriate isolation precautions can help prevent the spread of infection to other patients and healthcare workers.
Examples of Successful Implementation:
Several institutions have demonstrated the effectiveness of robust infection control programs. Kaiser Permanente's comprehensive infection control bundle has reportedly reduced surgical site infections by a remarkable 40%. The CDC's wound infection surveillance program in long-term care facilities provides valuable data for tracking infection rates and identifying areas for improvement. Furthermore, international wound care centers implementing silver-based dressings have reported reductions in infection rates by as much as 60%.
Actionable Tips for Patients and Healthcare Providers:
- Perform hand hygiene meticulously before and after any contact with a wound.
- Always use sterile dressings and techniques when changing dressings or performing other wound care procedures.
- Be vigilant in monitoring the wound for any signs of infection, such as increased pain, redness, swelling, warmth, or purulent drainage.
- Report any suspected signs of infection to your healthcare provider immediately.
- If prescribed antibiotics, take them exactly as directed and complete the entire course of treatment, even if symptoms improve.
- Avoid touching or picking at the wound.
- Keep the wound clean and dry.
When and Why to Use this Approach:
Infection prevention and control measures should be implemented from the moment a wound occurs and continued throughout the healing process. This proactive approach is essential for minimizing the risk of infection and promoting optimal healing outcomes. Whether it's a minor scrape or a complex surgical wound, adhering to these best practices is paramount for everyone involved in wound care, from patients and their families to healthcare professionals in all settings. By prioritizing infection prevention and control, we can significantly reduce the burden of wound infections and improve the lives of countless individuals.
4. Debridement and Tissue Management
Debridement and tissue management is a crucial element of wound care best practices, focusing on the systematic removal of dead, damaged, or contaminated tissue and foreign material from a wound. This process is essential for promoting healing and reducing the risk of infection. By optimizing the wound bed, debridement prepares the site for healing or closure, allowing the body's natural healing mechanisms to function more effectively. This practice significantly impacts wound care outcomes and is a cornerstone of modern wound management.
Debridement works by eliminating barriers that impede healing. Devitalized tissue provides a breeding ground for bacteria, hindering the formation of healthy granulation tissue and increasing the risk of infection. By removing this tissue, debridement reduces the bacterial load, stimulates the release of growth factors, and promotes cellular activity crucial for tissue repair. This, in turn, improves the effectiveness of topical treatments and reduces unpleasant wound odor, improving patient comfort and quality of life.
Several debridement methods cater to various wound types and patient conditions. Sharp/surgical debridement, performed by a skilled healthcare professional using a scalpel or other sharp instruments, offers rapid removal of necrotic tissue. Enzymatic debridement uses topical agents containing enzymes that break down dead tissue. Autolytic debridement harnesses the body's natural enzymes and is often facilitated by moisture-retentive dressings. Lastly, mechanical debridement involves methods like irrigation or wet-to-dry dressings to physically remove debris and dead tissue.
There are several benefits to debridement and tissue management, including: removing barriers to healing, reducing bacterial load, stimulating growth factor release and cellular activity, improving the effectiveness of topical treatments, and reducing wound odor and improving patient comfort. However, it is important to be aware of the potential drawbacks as well, which include temporary increased pain or bleeding, the need for skilled practitioners, and the fact that it can be time-consuming and require multiple sessions.
Numerous examples demonstrate the effectiveness of debridement. The University of Miami has reported a 45% improvement in diabetic foot ulcer outcomes through aggressive debridement protocols. European wound care centers have successfully integrated ultrasonic debridement technology, providing a less invasive approach. Even military field hospitals utilize rapid surgical debridement protocols, underscoring the importance of this technique across diverse healthcare settings.
The following infographic illustrates the basic three-step process involved in debridement:
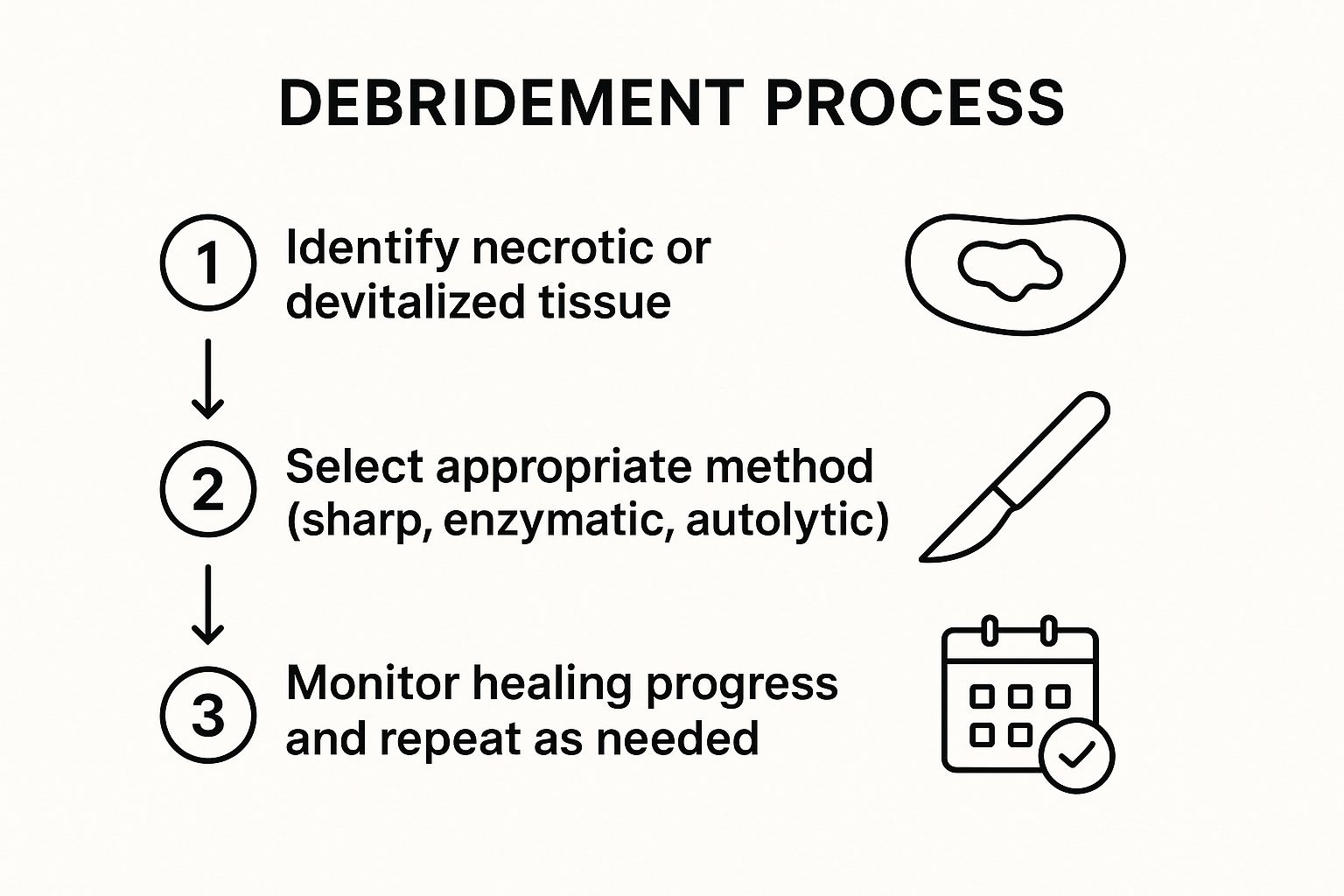
This infographic visualizes the cyclical nature of debridement, starting with the identification of necrotic tissue, followed by method selection and ongoing monitoring and repetition. The circular flow emphasizes the iterative nature of wound debridement, often requiring multiple sessions to achieve optimal results.
When considering debridement, several crucial tips should be kept in mind. Assessing the vascular supply before sharp debridement is essential to ensure adequate blood flow to the area. Appropriate pain management during procedures is vital for patient comfort. Selecting the appropriate debridement method should be based on the wound's characteristics and the patient's overall condition. Finally, continuous monitoring for bleeding and signs of viable tissue exposure is necessary for safe and effective treatment. Learn more about Debridement and Tissue Management.
Pioneering work by individuals like Dr. Vincent Falanga in wound bed preparation, along with organizations like the International Working Group on Wound Bed Preparation and companies like Misonix (developers of ultrasonic debridement technology), have significantly advanced the field of debridement and tissue management.
Debridement and tissue management earns its place among wound care best practices due to its crucial role in promoting healing, reducing infection risk, and ultimately improving patient outcomes. By understanding the different methods, benefits, and precautions associated with debridement, both healthcare providers and patients can make informed decisions about wound care.
5. Pressure Redistribution and Offloading
Pressure redistribution and offloading is a cornerstone of wound care best practices, especially for pressure ulcers and diabetic foot ulcers. This crucial technique focuses on minimizing or eliminating pressure, friction, and shear forces on wounds and areas susceptible to breakdown. By reducing these forces, we can prevent further tissue damage, promote healing, and significantly improve patient comfort. This approach is essential not only for treating existing wounds but also as a preventative strategy for at-risk individuals.

Pressure ulcers, also known as bedsores, develop when prolonged pressure restricts blood flow to the skin and underlying tissues. Similarly, diabetic foot ulcers are often exacerbated by pressure and friction from footwear and weight-bearing activities. Pressure redistribution and offloading addresses these issues by distributing weight evenly and reducing the forces that contribute to tissue breakdown. This is achieved through a combination of specialized equipment and strategic positioning techniques.
Several methods are employed to effectively redistribute pressure. Specialized support surfaces, such as low-air-loss mattresses and alternating pressure overlays, help to distribute weight more evenly across the body. These dynamic surfaces constantly adjust pressure points, promoting blood flow and reducing the risk of tissue damage. For individuals with foot ulcers, offloading devices like total contact casts, walking boots, and crutches are essential. These devices remove pressure from the affected area, allowing the ulcer to heal without further irritation. Regular turning and repositioning schedules are another critical component, particularly for bedridden or wheelchair-bound patients. Turning patients every two hours helps to alleviate pressure on bony prominences and promote circulation.
The benefits of pressure redistribution and offloading are substantial. This wound care best practice not only prevents further tissue damage and promotes healing in existing wounds but also plays a significant role in pain management. By reducing pressure, we can significantly alleviate discomfort associated with pressure ulcers and diabetic foot ulcers, improving the overall quality of life for patients. Furthermore, implementing preventative measures like pressure redistribution is a cost-effective strategy that can help avoid costly hospitalizations and complex wound care treatments down the line.
The successful implementation of pressure redistribution and offloading programs has been documented in various healthcare settings. Intermountain Healthcare, for instance, saw a 70% reduction in hospital-acquired pressure ulcers after implementing a comprehensive pressure ulcer prevention program. Diabetic foot clinics utilizing total contact casting have reported healing rates as high as 90%. These examples demonstrate the efficacy of these techniques when incorporated into a structured wound care plan.
While pressure redistribution and offloading offer numerous advantages, there are also challenges to consider. Consistent compliance from both patients and caregivers is crucial for success. Adhering to repositioning schedules, properly using offloading devices, and maintaining specialized equipment requires diligence and commitment. The cost of specialized equipment can also be a barrier for some individuals. Finally, some pressure redistribution and offloading methods may restrict patient mobility and independence, which can be a concern for some individuals.
To effectively implement pressure redistribution and offloading techniques, consider the following tips: Reposition patients at least every two hours or utilize dynamic support surfaces. Use heel protectors and cushioning for bony prominences like elbows, hips, and heels. Educate patients and their families on proper offloading techniques and the importance of adherence to the prescribed regimen. Thoroughly document repositioning schedules and compliance to ensure consistency and track progress.
Organizations like the National Pressure Ulcer Advisory Panel (NPUAP) and the European Pressure Ulcer Advisory Panel (EPUAP) have been instrumental in popularizing and standardizing pressure redistribution and offloading techniques. Companies like Hill-Rom have also contributed significantly to the field with innovations in therapeutic support surfaces. For those seeking more information, learn more about Pressure Redistribution and Offloading. By incorporating these best practices into your wound care approach, you can significantly improve patient outcomes and promote effective healing.
6. Nutritional Optimization: Fueling the Body's Healing Power
Nutritional optimization is a critical yet often overlooked aspect of wound care best practices. It involves the systematic assessment and management of a patient's nutritional status to ensure they have the necessary building blocks for effective wound healing. This approach recognizes that wounds, whether chronic or acute, place significant demands on the body's resources. By providing adequate protein, calories, vitamins, and minerals, we can empower the body to repair damaged tissue, fight infection, and ultimately achieve optimal healing outcomes. This makes nutritional optimization not just a supportive measure, but a fundamental pillar of comprehensive wound care.
The underlying principle of nutritional optimization is simple: providing the body with the right fuel. Wound healing is a complex metabolic process that requires increased energy expenditure and a readily available supply of nutrients. Protein, in particular, plays a crucial role in building new tissue, while calories provide the energy needed for cell regeneration and function. Specific vitamins and minerals, such as vitamin C, zinc, and arginine, also play essential roles in collagen synthesis, immune function, and blood vessel formation, all vital components of the healing process.
Ignoring nutritional needs can significantly impair wound healing and increase the risk of complications, especially infections. Malnourished individuals often experience delayed wound closure, increased susceptibility to infection, and prolonged hospital stays. Conversely, a well-nourished individual has a significantly improved capacity for tissue repair and a stronger immune system to combat infection, leading to faster healing and better overall outcomes. This is why nutritional optimization deserves its prominent place among wound care best practices.
A comprehensive approach to nutritional optimization involves several key features:
- Comprehensive nutritional assessment and screening: Using validated tools like the Malnutrition Screening Tool (MST) or the Nutritional Risk Screening (NRS 2002) allows healthcare professionals to identify patients at risk of malnutrition. These screenings should be conducted upon admission and regularly throughout the healing process.
- Adequate protein intake (1.2-1.5g/kg body weight): Protein is the cornerstone of tissue repair. Ensuring sufficient daily intake is crucial for optimal healing.
- Sufficient caloric intake to meet metabolic demands: Healing requires energy. Caloric needs should be calculated based on the patient's individual factors, including their age, activity level, and the severity of their wound.
- Supplementation with key nutrients: Specific nutrients like vitamin C, zinc, and arginine play targeted roles in the healing process and may need to be supplemented if dietary intake is insufficient.
The benefits of prioritizing nutritional optimization are numerous:
- Provides essential building blocks for tissue repair: Amino acids from protein are the raw materials for building new tissue.
- Supports immune function and infection resistance: Adequate nutrition strengthens the immune system, enabling the body to fight off infection and prevent complications.
- Improves overall patient outcomes and quality of life: Faster healing, reduced pain, and improved mobility contribute to a better quality of life for patients.
- Cost-effective intervention with multiple health benefits: By preventing complications and shortening hospital stays, nutritional optimization can actually reduce overall healthcare costs.
However, there are some challenges associated with nutritional optimization:
- Requires ongoing monitoring and adjustment: Nutritional needs can change throughout the healing process, requiring regular reassessments and adjustments to the plan.
- Patient compliance can be challenging: Some patients may struggle to meet their increased nutritional needs due to factors such as loss of appetite, difficulty swallowing, or dietary restrictions.
- May require specialized nutritional products: In some cases, specialized high-protein supplements or enteral nutrition may be necessary.
Successful implementations of nutritional optimization highlight its efficacy. The Cleveland Clinic reported a 35% reduction in wound complications after implementing routine malnutrition screening. European wound care centers have seen positive results with arginine supplementation protocols, and nursing homes using high-protein nutritional supplements have documented improved healing rates. These examples demonstrate the tangible benefits of incorporating nutritional optimization into wound care best practices.
Actionable tips for implementing nutritional optimization:
- Screen all wound patients for malnutrition using validated tools.
- Collaborate with registered dietitians for complex cases. They can develop individualized nutrition plans.
- Monitor albumin, prealbumin, and other nutritional markers to track the patient's nutritional status.
- Consider enteral nutrition for patients unable to meet needs orally.
- Educate patients and caregivers about the importance of nutrition in wound healing to improve compliance.
Leaders in the field of wound nutrition, including the Academy of Nutrition and Dietetics, the American Society for Parenteral and Enteral Nutrition (ASPEN), and experts like Dr. Nancy Collins, continue to advocate for the importance of nutritional optimization in wound care. By integrating these best practices into all levels of wound care, from primary care to specialized wound clinics, we can significantly improve healing outcomes and the overall quality of life for patients.
7. Patient Education and Self-Care Management
Patient education and self-care management are crucial components of wound care best practices. This comprehensive approach empowers patients and their caregivers to actively participate in the healing process, leading to improved outcomes and a better quality of life. By understanding wound care principles, self-monitoring techniques, and necessary lifestyle modifications, patients can take ownership of their health and contribute significantly to preventing complications and recurrences. This proactive involvement is essential for effective long-term wound management.
This approach works by equipping patients with the knowledge and skills they need to care for their wounds effectively outside of a clinical setting. It involves structured education programs that cover wound care basics, such as proper hygiene, recognizing signs of infection, and understanding the healing process. Hands-on training in dressing change techniques is also provided, allowing patients to confidently perform these procedures at home. Furthermore, education extends to teaching patients how to identify warning signs and symptoms that require immediate medical attention, empowering them to seek timely intervention and prevent potential complications. Finally, lifestyle modification counseling addresses underlying conditions that may contribute to wound development or impede healing, such as poor nutrition, smoking, or uncontrolled diabetes.
The benefits of incorporating patient education and self-care management into wound care best practices are numerous. Improved patient compliance with treatment plans is a key advantage, as educated patients are more likely to adhere to prescribed regimens and follow through with self-care activities. This, in turn, leads to better treatment outcomes and faster healing times. Moreover, proactive self-care can significantly reduce healthcare costs by minimizing the need for frequent clinic visits, emergency department visits, and hospitalizations. By preventing complications and recurrences, patients can avoid costly interventions and maintain their overall health. Perhaps most importantly, patient education empowers individuals and improves their quality of life. Taking an active role in their care fosters a sense of control and independence, reducing anxiety and improving overall well-being. Learn more about Patient Education and Self-Care Management
Several successful examples demonstrate the positive impact of patient education and self-care management. The Joslin Diabetes Center's patient education program has been instrumental in reducing diabetic foot complications by an impressive 50%. Similarly, community wound care services in the UK have implemented structured patient education initiatives, resulting in improved healing rates and reduced healthcare utilization. The increasing adoption of telehealth platforms has further expanded the reach of patient education, providing remote wound care education and monitoring to patients in underserved areas or those with limited mobility.
While the advantages are substantial, there are also some challenges associated with implementing effective patient education. It requires a significant time investment from healthcare providers, who must dedicate time to developing and delivering educational programs, conducting training sessions, and providing ongoing support. Patient learning capacity and compliance can also vary, and healthcare providers must tailor their approach to meet the individual needs and abilities of each patient. Cultural and language barriers can further impede effectiveness, highlighting the importance of culturally sensitive communication and the provision of translated materials.
To maximize the effectiveness of patient education and self-care management, consider the following tips:
- Use teach-back methods: After explaining a concept or procedure, ask the patient to explain it back to you in their own words to ensure comprehension.
- Provide written materials and visual aids: Supplement verbal instruction with clear, concise written materials and visual aids, such as diagrams or videos, to reinforce learning.
- Tailor education to patient's literacy level and cultural background: Consider the patient's literacy level and cultural background when developing educational materials and delivering instruction.
- Include family members and caregivers in education sessions: Engaging family members and caregivers in the education process provides additional support and ensures continuity of care.
Organizations like the Wound Ostomy and Continence Nurses Society (WOCN), the American Diabetes Association, and Healogics have been instrumental in popularizing and standardizing patient education programs for wound care. Their efforts have contributed significantly to raising awareness of the importance of patient education and promoting best practices in the field. By prioritizing patient education and self-care management, healthcare providers can empower patients to become active participants in their wound healing journey, leading to improved outcomes, reduced costs, and a better quality of life.
8. Multidisciplinary Team Approach: Optimizing Wound Care Best Practices
Effective wound care often requires more than a single healthcare professional. A multidisciplinary team approach, a cornerstone of wound care best practices, brings together a diverse group of specialists to provide comprehensive and coordinated care, ultimately enhancing healing outcomes and improving patient quality of life. This collaborative model addresses the multifaceted nature of wound healing, considering not just the physical wound but also the patient's overall health and well-being.
This approach involves the coordinated efforts of various healthcare professionals, each contributing their specialized knowledge and skills to the patient's care plan. This team may include physicians (primary care, vascular surgeons, plastic surgeons), nurses (wound care certified nurses, registered nurses), wound specialists, dietitians, physical therapists, occupational therapists, and other specialists as needed. For instance, a patient with a diabetic foot ulcer might benefit from the expertise of an endocrinologist and a podiatrist, in addition to the core wound care team. This integrated approach ensures all aspects of wound healing are considered, from managing blood sugar levels and optimizing nutrition to addressing pain management and mobility issues.
The multidisciplinary team operates through regular meetings and case conferences, fostering open communication and collaboration among the members. These discussions allow for the sharing of information, perspectives, and treatment strategies, ensuring a unified approach to patient care. Coordinated care plans are developed, addressing not only the wound itself but also factors like nutrition, pain management, infection control, and patient education. For complex or non-healing wounds, specialist consultations are readily available, offering access to advanced treatments and expertise.
Several successful examples demonstrate the power of a multidisciplinary team approach in wound care. The Mayo Clinic's integrated wound care team, for instance, has reported a remarkable 60% reduction in amputation rates among patients with complex wounds. Similarly, the Geisinger Health System saw a 40% improvement in chronic wound healing rates after implementing a multidisciplinary approach. The VA Medical Centers have also embraced this model, establishing team-based diabetic foot care programs with demonstrably positive outcomes. These successes highlight the effectiveness of this approach in improving wound healing and preventing complications.
Benefits of a Multidisciplinary Approach:
- Comprehensive Care: Addresses all factors affecting wound healing, including medical, nutritional, and psychosocial aspects.
- Improved Communication: Facilitates seamless communication between healthcare providers, reducing the risk of fragmented care and errors.
- Enhanced Clinical Outcomes: The combined expertise of multiple specialists leads to better treatment decisions and improved healing rates.
- Patient Empowerment: Patients are actively involved in their care plan, leading to increased compliance and better self-management.
- Support and Education: Provides ongoing support and education for both patients and healthcare team members.
Challenges of a Multidisciplinary Approach:
- Coordination and Communication: Requires substantial effort to coordinate schedules and ensure effective communication between team members.
- Cost: May involve higher initial healthcare costs due to the involvement of multiple specialists.
- Logistical Challenges: Scheduling regular team meetings and ensuring the availability of all members can be challenging.
Tips for Implementing a Multidisciplinary Team Approach:
- Establish clear roles and responsibilities: Ensure each team member understands their role and responsibilities within the team.
- Utilize electronic health records: Leverage technology to facilitate communication and information sharing among team members.
- Hold regular case conferences: Schedule regular meetings to discuss complex cases and develop coordinated care plans.
- Include patients and families: Engage patients and their families as active participants in the care team, empowering them to take ownership of their health.
When facing a complex or non-healing wound, a multidisciplinary approach to wound care best practices is highly recommended. It offers a comprehensive and coordinated strategy that addresses all factors influencing healing. While it requires significant coordination and may involve higher initial costs, the potential benefits in terms of improved healing outcomes, reduced complications, and enhanced patient quality of life make it a valuable investment. You can Learn more about Multidisciplinary Team Approach and explore the reasons why home health care is an essential component in some cases. Organizations such as the Institute for Healthcare Improvement (IHI) and the Wound Healing Society, along with pioneers like Dr. David Armstrong in the field of diabetic foot care, have championed this team-based approach, solidifying its place as a best practice in modern wound care.
8 Key Wound Care Practices Comparison
| Best Practice | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Comprehensive Wound Assessment | High – requires skilled practitioners and multiple tools | Moderate – specialized instruments and documentation | Accurate treatment planning and healing monitoring | Initial wound evaluation and ongoing monitoring | Enables evidence-based care; identifies healing barriers |
| Moisture Balance Management | Moderate – frequent dressing changes and monitoring | Moderate to high – advanced dressings can be costly | Faster tissue repair, reduced pain, prevention of maceration | Wounds with varying exudate levels needing moisture control | Accelerates healing; protects periwound skin |
| Infection Prevention and Control | High – constant vigilance, strict protocols | High – sterile materials and antimicrobials | Reduced infection rates, fewer complications | All wounds at risk of infection, especially surgical wounds | Prevents sepsis; lowers healthcare costs |
| Debridement and Tissue Management | High – requires clinical skill and multiple sessions | Moderate – tools and possible procedural costs | Removal of necrotic tissue, improved healing environment | Chronic, necrotic, or contaminated wounds | Removes healing barriers; stimulates tissue regeneration |
| Pressure Redistribution and Offloading | Moderate – ongoing patient/caregiver compliance | Moderate to high – specialized equipment needed | Prevention of tissue damage, improved healing | Pressure ulcers, diabetic foot ulcers | Prevents deterioration; enhances patient comfort |
| Nutritional Optimization | Moderate – requires ongoing assessment and dietary support | Moderate – specialized nutritional products possible | Improved tissue repair and immune support | Patients with malnutrition or increased metabolic needs | Supports healing systemically; cost-effective intervention |
| Patient Education and Self-Care Management | Moderate – significant time for education and follow-up | Low to moderate – educational materials and sessions | Increased compliance, reduced complications | All patients, especially chronic wound sufferers | Empowers patients; decreases healthcare utilization |
| Multidisciplinary Team Approach | High – coordination and communication intensive | High – multiple specialists involved | Comprehensive care, improved complex wound outcomes | Complex or chronic wounds requiring multi-specialty input | Enhances outcomes; reduces care fragmentation |
Taking the Next Step in Wound Care
Proper wound care is crucial for preventing complications, improving patient comfort, and facilitating faster healing. This article has outlined eight wound care best practices, encompassing comprehensive wound assessment, moisture balance management, infection prevention and control, debridement and tissue management, pressure redistribution and offloading, nutritional optimization, patient education and self-care management, and the importance of a multidisciplinary team approach. Mastering these wound care best practices is essential for healthcare professionals to deliver effective care and for patients to actively participate in their healing journey. By prioritizing these strategies, we can significantly reduce healing times, minimize scarring, and prevent long-term complications that can impact a patient's quality of life.
From accurate assessments to appropriate dressings and patient empowerment through education, every step plays a vital role in optimizing outcomes. Remember, effective wound care is a collaborative process. By working together and incorporating these wound care best practices, patients and healthcare providers can achieve the best possible results.
For those seeking additional support and personalized guidance in implementing these wound care best practices, Rapid Wound Care offers comprehensive, at-home services. Specializing in chronic wounds, pressure injuries, and diabetic ulcers, Rapid Wound Care provides expert care tailored to your individual needs. Learn more about how Rapid Wound Care can help you on your path to recovery by visiting Rapid Wound Care today.

