Why Traditional Wound Assessment Falls Short Today
Imagine two nurses examining the same wound. One meticulously measures and documents a 3cm x 2cm area, while the other, using the same tools, records it as 4cm x 3cm. This discrepancy, though seemingly small, can have big consequences. It's like two chefs using the same ingredients but getting wildly different results – something's off with the recipe.
Traditional wound assessment, relying solely on rulers and the naked eye, is inherently subjective. Think of trying to describe a color to someone without using a color chart – your "cherry red" might be their "crimson." This subjectivity makes it hard to accurately track healing progress and can lead to inconsistencies in treatment.
The complexity of wound healing itself contributes to the challenge. The image below, from the Wikipedia page on Wound Healing, illustrates this:
Just like a building project has distinct phases – foundation, framing, finishing – wound healing progresses through specific stages. Accurate assessment isn't just about measuring size; it's about understanding where the wound is in its healing journey. This informs treatment decisions, ensuring the right intervention at the right time.
Traditional methods often fall short in capturing crucial details like wound depth and volume. It's like trying to understand a story by only reading the headlines – you miss the nuance and depth. Furthermore, accurately identifying tissue type is crucial, yet difficult with conventional methods. Mistaking healthy granulation tissue for slough, for example, can lead to unnecessary and potentially harmful interventions.
The limitations of traditional assessment highlight the need for a more precise and objective approach. Modern wound assessment tools offer just that. You might find this interesting: What is mobile wound care and why is it important? Access to advanced assessment tools is a cornerstone of mobile wound care's benefits. These tools empower clinicians with the detailed data needed to make informed decisions, predict healing trajectories, and tailor treatment plans to each patient's unique needs. This shift towards precision wound care is essential for optimizing patient outcomes.
Digital Measurement: From Guesswork To Precision
Remember trying to measure a wound with a ruler? It's like tracing the edge of a puddle – your measurement changes depending on your angle. This traditional method often leads to inconsistencies between clinicians, making it difficult to track healing accurately.
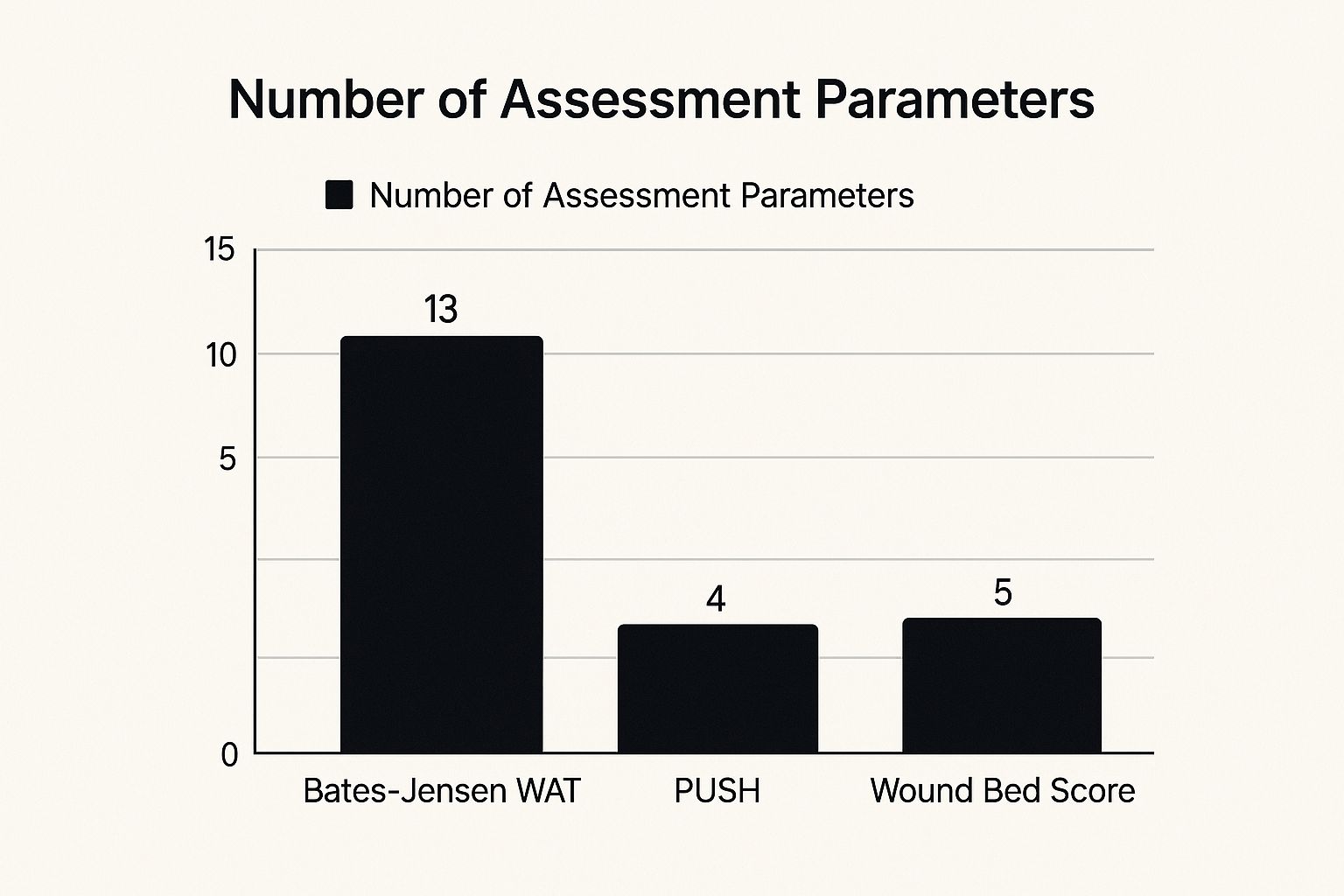
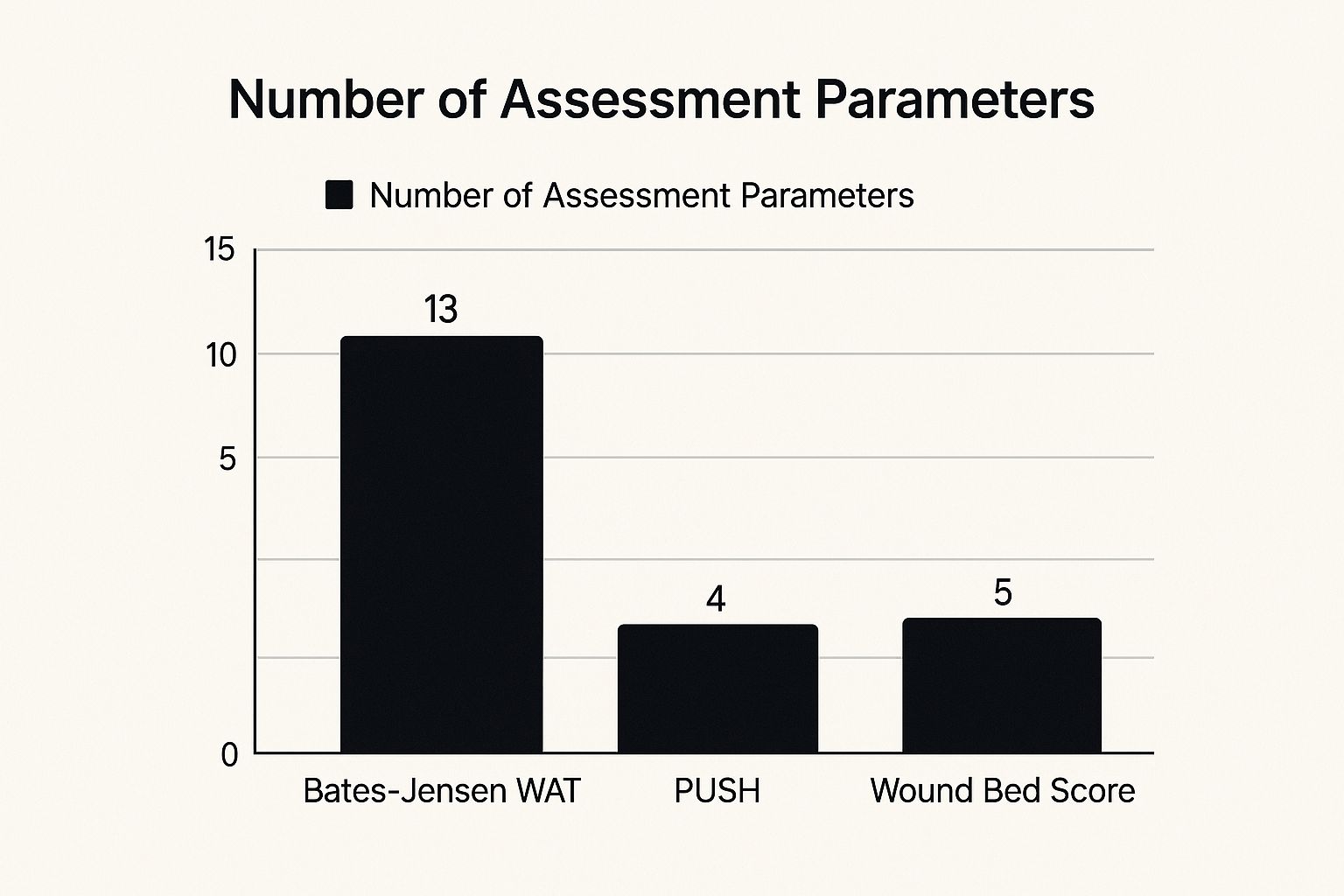
This infographic highlights the variability in traditional assessments. The Bates-Jensen WAT uses 13 parameters, the PUSH tool uses 4, and the Wound Bed Score uses 5. These differences demonstrate the potential for inconsistency when relying on manual methods.
Embracing Digital Precision
Digital wound assessment tools offer a much-needed upgrade. Imagine switching from a hand-drawn map to GPS – you gain accuracy and reliability. These tools utilize technologies like 3D imaging and laser scanning to capture precise measurements, eliminating the guesswork of manual assessments.
For example, 3D imaging creates a digital "mold" of the wound, allowing for accurate volume calculations – a key factor often missed with traditional methods. This allows clinicians to track volume changes over time, providing a more complete picture of healing progress.
This screenshot from WoundSource showcases the growing emphasis on advanced wound care resources. The platform offers valuable information and tools for professionals in the field.
The Rise of Digital Wound Measurement
The increasing prevalence of chronic wounds, coupled with advancements in technology, is fueling the growth of the digital wound measurement market. In 2024, this market generated about $1,080.7 million in revenue, and it's projected to reach $1,887.5 million by 2035, growing at a CAGR of 5.2%. Learn more about this growing market.
Even smartphone apps are getting in on the action, bringing digital measurement capabilities to point-of-care settings. These apps can analyze wound images, track healing, and even suggest treatment options. For more tips on wound healing, check out our guide on how to heal deep wounds faster.
To help you navigate the world of digital wound measurement, we've compiled a comparison of popular tools:
Digital Wound Measurement Tools Comparison
Comparison of popular digital measurement tools showing features, accuracy levels, and clinical applications
| Tool Type | Measurement Accuracy | Key Features | Best Use Cases | Cost Range |
|---|---|---|---|---|
| (Example) 3D Wound Imaging System | +/- 1mm | Volume calculation, surface area analysis, depth measurement | Complex wounds, surgical wounds, research studies | High |
| (Example) Smartphone App with Planimetry | +/- 3mm | Area and perimeter measurement, image storage, progress tracking | Routine wound assessments, telemedicine, home care | Low |
| (Example) Laser Scanner | +/- 2mm | Precise surface area and perimeter, 3D modeling | Burns, ulcers, reconstructive surgery | Medium |
This table highlights the various options available, from high-precision systems to accessible smartphone apps. The choice depends on the specific needs of the clinical setting and the types of wounds being assessed.
The ability to accurately and quickly assess wounds with digital tools is transforming wound care, leading to better treatment plans and improved patient outcomes.
Building Your Assessment Framework That Actually Works
Effective wound assessment isn't about randomly poking and prodding. It needs a systematic approach, much like planning a road trip. You wouldn't just start driving without a map, would you? A structured framework acts as your roadmap, guiding you through the assessment and ensuring you gather all the essential information.
The TIME Framework: A Clinical Roadmap
The TIME framework is a widely used approach, and it's surprisingly easy to remember. TIME stands for Tissue, Infection/Inflammation, Moisture balance, and Edge of wound. Think of these as the four cardinal directions of wound assessment. Each component provides crucial clues, guiding your clinical decisions.
- Tissue: What's the wound bed composed of? Is it healthy, vibrant granulation tissue, or is there dead, necrotic tissue present? It's like assessing the foundation of a house – is it solid or crumbling?
- Infection/Inflammation: Are there telltale signs of infection, like redness, swelling, or increased pain? This is similar to checking for leaks or cracks in the house's structure.
- Moisture balance: Is the wound too dry, too wet, or just right? Maintaining the Goldilocks zone of moisture is like ensuring proper ventilation – essential for a healthy environment.
- Edge of wound: Is the wound's perimeter expanding or shrinking? Are there signs of undermining or tunneling, like hidden passages around the house?
Adapting Frameworks for Different Wound Types
Just as you'd adjust your driving route based on the terrain – navigating mountains versus flatlands – you adapt your assessment framework to the specific wound type. A simple surgical wound might need a quick check-up, while a complex chronic ulcer requires a more thorough investigation.
This screenshot from the Wound Care Society website highlights the crucial role of education and readily available resources in wound care. The society provides a treasure trove of information for clinicians, constantly pushing for better assessment and treatment.
The existence of these resources underscores the growing emphasis on evidence-based wound care. This aligns perfectly with the goal of using assessment tools to make informed, data-driven decisions that lead to better patient outcomes.
Customizing for Patients and Settings
Patient-specific factors like age, other medical conditions, and even lifestyle also influence your assessment approach. A wound in a patient with diabetes, for example, requires different considerations than a pressure injury in an elderly patient.
Your clinical setting also matters. A bustling emergency room demands a different approach than a specialized wound clinic. For more on managing wounds at home, check out our article on At-Home Wound Care. The key is to develop a framework that's both comprehensive and adaptable.
This adaptability ensures consistent, high-quality assessments, leading to more effective treatments and improved healing. A solid framework boosts your clinical confidence and lays the groundwork for evidence-based practice.
To help organize your assessment, consider the following table:
Wound Assessment Framework Components
| Assessment Category | Key Parameters | Clinical Significance | Documentation Methods |
|---|---|---|---|
| Tissue | Type (granulation, necrotic, slough), color, texture | Indicates wound healing phase, potential for infection | Photography, written descriptions, wound tracing |
| Infection/Inflammation | Redness, swelling, warmth, pain, exudate (pus), odor | Determines the presence and severity of infection | Wound cultures, laboratory tests, visual assessment documentation |
| Moisture Balance | Amount and type of exudate (serous, sanguineous, purulent), dryness, maceration | Impacts healing rate and risk of infection | Descriptive terms (dry, moist, wet), measurement of exudate |
| Edge of Wound | Advancement, recession, undermining, tunneling, epithelialization | Shows wound progression or complications | Wound measurements, photography, descriptive terms |
This table summarizes the core components of a thorough wound assessment and highlights the importance of meticulous documentation. By systematically evaluating each category, you can create a targeted treatment plan and monitor progress effectively.
AI-Powered Assessment: Your New Clinical Partner
Imagine wound care not as a field relying on subjective estimations, but one driven by data and precision. That's the promise of Artificial Intelligence (AI). It's not about replacing clinicians, but giving them a powerful new tool. Think of it like a seasoned detective getting cutting-edge forensic equipment – their experience combined with technology becomes incredibly effective.
Machine Learning: The Engine of AI Assessment
At the core of AI-powered wound assessment tools are machine learning algorithms. Picture these algorithms as diligent students, tirelessly poring over mountains of data: thousands of wound images, patient records, and treatment outcomes. They sift through this information, identifying patterns and connections that might be missed by the human eye. This allows the AI to learn from a far wider range of cases than any single clinician could possibly encounter, developing a deep understanding of wound characteristics and how they heal.

This image from HealthTechZone shows how technology and healthcare are increasingly intertwined. It reflects a larger trend: healthcare solutions are becoming more data-driven and technologically advanced.
AI in Action: Real-World Applications
AI-powered tools are already changing clinical practice. Imagine a smartphone app that analyzes a wound photo and instantly identifies its type – diabetic ulcer, pressure injury, surgical site infection – with incredible accuracy. This quick assessment guides initial treatment decisions, ensuring patients get the right care fast. Beyond that, advanced imaging systems use AI to automatically track healing progress. They meticulously measure changes in wound size, depth, and tissue composition over time, eliminating the guesswork of manual measurements and providing objective data to evaluate treatment success.
The use of AI in wound care is expanding rapidly. The AI in wound care market is expected to jump from $3.32 billion in 2025 to $7.65 billion by 2030, a compound annual growth rate (CAGR) of 18.17%. Discover more insights about the growing market.
Addressing Concerns and Maintaining Clinical Expertise
With AI's rise in wound care come important questions. Concerns around data privacy, the need for specialized training, and the possibility of technology overshadowing clinical judgment are all valid and need careful thought. Remember, the aim of AI isn’t to replace human expertise, but to enhance it. Clinicians remain crucial for interpreting AI insights, creating individual patient treatment plans, and providing the human touch so vital in healthcare. Home Health Wound Care Patient Outcomes offers further insights. The key is finding the right balance: using the strength of AI while keeping clinical judgment at the heart of patient care. This collaborative approach ensures patients benefit from both advanced technology and the experience of skilled professionals.
Choosing Tools That Fit Your Reality
Picking the right wound assessment tools can feel overwhelming. There are so many options out there! How do you separate the truly helpful tools from the expensive gadgets that don't deliver? This section gives you a practical guide to choosing wound assessment tools that will actually improve your clinical practice. We'll look at how other healthcare organizations successfully built their assessment programs, including the unexpected challenges they faced and the clever solutions they came up with.
Matching Tools to Your Unique Needs
Think about buying a car based only on its flashy color. You might end up with something that doesn't actually suit your needs. Choosing wound assessment tools is similar. You need to carefully consider your specific situation. Learn to evaluate tools based on factors like the types of patients you see, your clinical setting, your budget, and your team's skills – not just the marketing hype. A busy emergency room, for example, needs speed, while a specialized wound clinic needs precision.
This screenshot from Medical Device Network shows just how many medical devices are available. It highlights why it's so important to be picky when choosing new tools, making sure they fit your specific clinical requirements.
Learning From Real-World Experiences
We'll use real-world case studies to explore how different healthcare settings approach tool selection. We'll see how a busy ER might choose a portable, rapid imaging system for quick assessments, while a wound clinic might invest in a high-resolution 3D imaging system for detailed analysis. Consider the global market for digital wound measurement devices. Fueled by things like the rise in traumatic injuries and the increasing use of 3D measurement, this market is expected to reach $2.75 billion by 2025, growing at a 7.3% CAGR from $2.56 billion in 2024. You can find more information about this growing market here.
Avoiding Common Pitfalls and Overcoming Resistance
Bringing in new tools often meets resistance. Clinicians might be comfortable with their current methods, even if they're less accurate. Implementation can also be tricky, with potential problems like insufficient staff training or incompatibility with existing electronic health records. We'll discuss these common roadblocks and offer solutions based on what has and hasn't worked for other healthcare providers. You might also find this helpful: Pressure Ulcer Treatment Home Care for more insights into how home care utilizes specialized tools.
Making Informed Decisions for Better Outcomes
Our goal is to help you make smart decisions that benefit both your patients and your organization. This means choosing tools that improve patient care, make the best use of resources, and avoid expensive mistakes. By learning from others' experiences and taking a practical approach, you can confidently choose wound assessment tools that truly make a difference. This proactive approach helps you avoid being swayed by marketing and instead focus on tools that meet your actual needs.
Choosing the right tools isn't just about buying technology; it's about building a system that improves patient care. This involves assessing your current practices, understanding your particular needs, evaluating the available options, and planning for smooth implementation. It's about investing in tools that enable your team to provide the best possible care, resulting in better patient outcomes and greater clinical efficiency.
Real Success Stories From The Field
Theory is great, but nothing beats seeing these wound assessment tools in action. Let's dive into some real stories from healthcare professionals who transformed their wound care practices.
Rural Clinic Improves Chronic Wound Healing
Imagine a rural clinic struggling with wound assessments. Simple rulers and visual guesswork weren't cutting it, leading to inconsistencies in care and slow healing. They knew they needed a change.
After adopting a structured assessment protocol with digital photography and a mobile app for wound measurement, things started to look up. Accurate measurements meant they could truly track healing progress and fine-tune treatment plans. Within six months, their chronic wound healing rates jumped by 15%. It wasn't just about the tech; it was about empowering the team with solid data, boosting their confidence, and ultimately improving patient outcomes.
Urban Hospital Slashes Infection Rates
An urban hospital faced a different challenge: high infection rates in their wound care unit. Traditional assessments often missed subtle signs of trouble.
By bringing in digital monitoring tools to track temperature changes and other physiological indicators, they could suddenly spot early infection signs they'd previously missed. This early detection meant quicker intervention, and within a year, they slashed infection rates by 20%. This story shows how technology can supercharge clinical judgment, leading to real improvements in patient safety.
Home Healthcare Agency Revolutionizes Care Coordination
Think about the challenges of a home healthcare agency – clinicians spread out, potentially using different assessment methods, making it tough to track progress and ensure everyone's on the same page.
This agency tackled the problem head-on by adopting a mobile assessment application. This standardized their data collection and opened up real-time communication between clinicians. The result? Improved care coordination and a 10% reduction in hospital readmissions. This highlights how powerful standardized assessments and clear communication can be, especially in a complex setting like home healthcare.

This screenshot from the Wound Care Journal website shows the wealth of information available to wound care professionals. The range of topics emphasizes the field's growing focus on research and innovation, driving improvements in wound assessment and treatment. It also highlights the importance of staying up-to-date, showing clinicians how to integrate the latest findings and technologies into their practice.
These aren't just success stories; they're examples of how the right tools and a willingness to adapt can dramatically improve patient care. They show what's possible when clinical expertise meets modern technology, leading to better outcomes in wound care. These real-world experiences offer practical insights and encouragement for anyone looking to elevate their wound care practice. They prove that with planning, training, and support, new assessment methods can truly make a difference.
Your Action Plan For Assessment Excellence
Think of wound assessment like building a house. You wouldn't start slapping boards together without a blueprint, would you? The same goes for wounds. A structured approach is key to success, leading to better results for your patients and more confidence in your own skills.
Evaluate Your Current Assessment Practices
First, take a look at your current methods. It’s like checking the foundation of your house – crucial for stability. What tools are you using? Are they consistently giving you accurate measurements? Is everyone on your team getting the same readings? An honest self-assessment is the first step.
Identify Your Specific Needs
Just as different houses need different blueprints, different clinical settings need different tools. Are you in a busy ER or a specialized wound clinic? What's your patient population like? What's your budget? Considering these factors helps you pick the right tools for the job.
Explore and Select Appropriate Wound Assessment Tools
Now comes the fun part: exploring the options! From digital imaging systems like Swift Medical to AI-powered apps, modern tools offer amazing capabilities. It's like choosing the right materials for your house – quality matters. Remember your needs assessment from the previous step. Which tools best fit your specific situation?
Develop a Realistic Implementation Timeline
Introducing new tools takes time and planning, much like scheduling the different stages of building a house. Create a timeline that fits your schedule and budget. Break it down into smaller, manageable steps. Don’t forget to include staff training and integration with your existing systems.
Measure Success and Track Improvements
Once you've rolled out the new tools, it's time to track their impact. Are wounds healing faster? Are infections going down? It’s like inspecting the finished house – making sure everything is up to code. Regularly monitor your progress and be ready to make adjustments along the way.
Address Concerns and Maintain Momentum
Change can be tough. Some clinicians might be hesitant to adopt new methods. Address their concerns and provide ongoing support. Just like a house needs regular maintenance, your assessment practices need consistent attention. Celebrate your wins and keep the momentum going even after the initial excitement fades.
This action plan is your blueprint for assessment excellence. By following these steps, you can improve patient care and boost your own clinical expertise and confidence.
Ready to take your wound care practice to the next level? Explore the services offered by Rapid Wound Care and see how their personalized approach can transform your patients’ healing journey. They provide comprehensive at-home wound care, using advanced therapies and a patient-focused approach to promote faster healing and overall well-being.

