Choosing the right dressing is far more than just slapping a bandage on a cut. It's about hand-picking a specialized tool that actively partners with the body's own incredible healing process. The world of wound dressings is vast, ranging from the simple gauze in your first-aid kit to advanced bioactive materials, each engineered for a specific job.
Why The Right Wound Dressing Matters

Think of a wound as a delicate ecosystem. Like a gardener tending to a prize-winning rose, you need to create the perfect environment for it to flourish. You wouldn't use sandy, dry soil for a plant that needs rich, moist earth. It's the same with wounds.
The dressing you select acts as that carefully prepared soil. It's there to provide the ideal balance of moisture, protection from the elements, and active support for healing. This choice is critical. Using the wrong dressing can stall the healing process, cause unnecessary pain during changes, or even open the door to serious infection. The ultimate goal is to perfectly match the dressing's features to the wound's needs—a task that becomes even more important as the wound evolves through its healing stages.
To make the right choice, you first have to understand what you're treating. Getting familiar with the fundamental differences between the 6 types of wounds is the essential first step.
The Growing Need for Specialized Dressings
The demand for sophisticated wound care is more pressing than ever, driven largely by the increase in chronic conditions like diabetes and vascular disease that often lead to complex wounds. The market for these specialized products tells the story. The global advanced wound dressing market is on a steep upward trajectory, projected to grow from around USD 6.25 billion in 2025 to an estimated USD 8.74 billion by 2035.
This isn't just about money; it represents a fundamental shift in how we approach healing. We've moved from passively covering wounds to actively managing them. Modern dressings are engineered marvels designed to:
- Manage moisture levels, either by wicking away excess fluid (exudate) or by donating moisture to a dry wound bed.
- Protect the wound by forming a barrier against bacteria and other outside contaminants.
- Promote autolytic debridement, which is the body's natural, gentle way of clearing away dead tissue.
- Minimize pain and prevent damage to the delicate new skin when the dressing is changed.
The core principle of modern wound care is creating an optimal healing environment. The right dressing isn't just a barrier; it's an active participant in the recovery process, interacting with the wound to facilitate cellular repair and tissue regeneration.
To help you get your bearings in this complex field, we've put together a simple table that breaks down the main dressing categories. Think of it as your starting point—a quick-reference map before we explore the unique characteristics of each type in detail.
Quick Guide to Wound Dressing Categories
| Dressing Category | Primary Function | Best For |
|---|---|---|
| Gauze | Protection, absorption, packing | Minor cuts, post-surgical sites, covering other dressings |
| Transparent Films | Creates a waterproof barrier | Superficial wounds, IV sites, protecting at-risk skin |
| Foams | High absorption, cushioning | Moderately to heavily exuding wounds, pressure injuries |
| Hydrocolloids | Moist healing, autolytic debridement | Light to moderate exudate, burns, pressure ulcers |
| Hydrogels | Donates moisture | Dry or necrotic wounds, minor burns, painful wounds |
| Alginates & Hydrofibers | Very high absorption | Heavily exuding or bleeding wounds, deep cavity wounds |
| Antimicrobials | Reduces bacterial load | Infected or high-risk wounds |
| Collagen | Stimulates tissue growth | Chronic, stalled, or non-healing wounds |
This table provides a high-level snapshot. Now, let's zoom in and really get to know each of these wound care powerhouses, so you can confidently choose the right tool for the job.
Understanding Traditional Wound Dressings
When you picture wound care, what's the first thing that comes to mind? For most people, it's the simple gauze pads and adhesive bandages found in every medicine cabinet. These are what we call traditional dressings, and they represent the very foundation of wound management. Even with all the incredible advancements in modern medicine, these classics still have an important job to do.
Think of traditional dressings as the reliable old pickup truck of the wound care world. They aren't fancy, but they get the job done. Their main roles are straightforward: protection and absorption. They act as a simple shield to keep dirt and germs out of a wound while soaking up minor amounts of fluid (what we call exudate). They're at their best when dealing with simple, clean wounds that aren't draining much.
A perfect example is using a standard gauze dressing to cover a fresh, minor surgical incision or to protect a small scrape that's stopped bleeding.
The Role of Gauze and Basic Dressings
Gauze is a remarkably versatile tool. You can place it directly on a wound as a primary dressing, or you can use it as a secondary layer to hold another dressing securely in place. It's breathable, easy to find, and doesn't cost much, which makes it a go-to choice in many scenarios.
However, that simplicity comes with some real downsides. Perhaps the biggest problem with traditional gauze is that it can dry out and weld itself to the wound bed. When that happens, pulling it off is not only painful but can rip away the delicate new tissue that the body has just created. This can stall the healing process, essentially re-injuring the wound every time you change the dressing. This very issue is what drove the innovation of more advanced types of wound dressings.
A core challenge with traditional dressings is maintaining a balanced healing environment. While they offer protection, their tendency to adhere to the wound can disrupt the very tissue the body is working so hard to build, highlighting the need for dressings that support, rather than hinder, the natural healing process.
Knowing When to Use Traditional Options
So, when are these old-school dressings the right choice? They shine in very specific situations where the wound just needs basic coverage without any complex moisture needs.
- Minor Abrasions and Cuts: For clean scrapes and small cuts with little to no drainage, a simple adhesive strip or a small gauze pad is often all you need.
- Post-Surgical Incision Protection: They are commonly used to cover clean, stitched surgical sites, protecting them from rubbing and contamination.
- Secondary Dressings: Gauze rolls and pads are fantastic for securing more advanced primary dressings or for adding an extra layer of cushioning and absorption on top.
These dressings are the starting point for understanding wound care. They handle the simple stuff well, but their limitations quickly become apparent with more complicated injuries. If you're dealing with a more significant injury, our guide on how to heal deep wounds faster offers deeper insights into more effective methods. Understanding where traditional dressings come up short is key to appreciating why the next categories of interactive and advanced dressings are so critical for modern wound management.
How Interactive Dressings Accelerate Healing
https://www.youtube.com/embed/ynlJC0zkjDY
For a long time, the go-to advice was to let a wound "breathe" and keep it dry. We’ve since learned that this actually slows down healing. When a wound dries out, a hard scab forms, which physically blocks new, healthy cells from growing across the wound bed. The real game-changer was the move to moist wound healing—the understanding that our cells need a balanced, hydrated environment to repair and regenerate properly.
This is exactly where interactive dressings shine. They don’t just sit there and cover a wound; they actively work with the wound bed to create the perfect healing conditions. Think of them as intelligent materials that manage the environment, either by soaking up excess fluid or by donating moisture to a dry wound.
The value of these dressings is clear in the market. In 2024, the interactive wound dressing market was valued at around USD 4.43 billion, and it's projected to climb to USD 4.67 billion by 2025. This isn't just a trend; it's a direct response to the growing need for effective treatments for chronic wounds.
The Power of Hydrocolloids
Hydrocolloid dressings are a classic example of this interactive approach. These dressings are made with gel-forming agents, like pectin or gelatin, mixed into an adhesive. When you place one on a wound with light to moderate drainage, the dressing absorbs the fluid (called exudate) and turns it into a soft, moist gel right over the wound.
This gel does two very important things:
- It maintains a consistently moist environment, which helps new tissue grow much faster.
- It supports autolytic debridement, which is the body's natural and gentle way of breaking down and washing away dead tissue without harming the healthy stuff.
Because the gel stays contained within the dressing, hydrocolloids are waterproof and form a great barrier against bacteria. They're a solid choice for non-infected pressure injuries, minor burns, and other shallow wounds, especially since they can stay on for several days, giving the wound uninterrupted time to heal.
Donating Moisture with Hydrogels
But what if the wound is too dry? A dry wound covered in dead, or necrotic, tissue is a major roadblock to healing. In these cases, you need a dressing that gives moisture instead of taking it away. That's the job of hydrogel dressings.
These dressings are mostly water—often over 90%—held in a gel. Think of it like giving a thirsty plant a drink. By donating moisture to the wound bed, hydrogels rehydrate and soften the dry tissue, making it much easier for the body to clear it away. As a bonus, this process is incredibly soothing and can bring significant pain relief to the patient.
Hydrogels are like a purpose-built cool compress that also actively helps with healing. They are the perfect choice for dry wounds, wounds with dead tissue, radiation skin damage, and painful minor burns, offering both moisture and immediate comfort.
The Clear Advantage of Transparent Films
Sometimes, the most critical feature of a dressing is simply being able to see through it. Transparent film dressings are thin, see-through polyurethane sheets with an adhesive backing. While they don't absorb much fluid, their unique properties make them essential for specific situations.
Their main benefits are:
- Constant Monitoring: They allow a clinician to check on a wound or an IV site without having to take the dressing off, which cuts down on the risk of contamination.
- Waterproof Barrier: They shield the site from bacteria and water but are still permeable enough to let oxygen reach the skin.
- Friction Reduction: They can be placed over bony areas, like elbows or heels, to protect fragile skin from friction and shear.
These films are ideal for securing IV catheters, covering superficial wounds like skin tears, and acting as a secondary dressing over something else. The ability to watch the healing process without frequent dressing changes is a huge advantage, and it’s a cornerstone of good wound management. If you want to learn more about how this fits into a larger care plan, our article on how home wound care speeds up recovery offers some great insights.
Choosing Advanced Dressings for Complex Wounds
When you're dealing with a wound that's deep, draining heavily, or just stubbornly refusing to heal, standard bandages won't cut it. This is where advanced wound dressings come into play. Think of them as the special forces of wound care—highly specialized tools designed to tackle the toughest clinical challenges and actively support the healing process.
Foam Dressings: The Ultimate Shock Absorber
For wounds that produce a lot of fluid, known as exudate, foam dressings are a fantastic first line of defense. Made from materials like polyurethane, these dressings are incredibly absorbent. Picture a high-tech sponge for a wound; it wicks excess moisture away from the wound bed and locks it inside the dressing. This simple action is crucial—it prevents the surrounding healthy skin from getting waterlogged and breaking down, all while keeping the wound itself perfectly moist for healing.
Their soft, cushioned structure also provides excellent protection, making them a go-to for safeguarding bony areas prone to pressure injuries.
Alginate Dressings: For Deep and Heavily Draining Wounds
What about wounds with even more drainage, or those with significant depth and tunneling? That’s a job for alginate dressings. These remarkable dressings are derived from natural brown seaweed and are true workhorses. In fact, an alginate can soak up to 20 times its own weight in fluid.
When an alginate dressing meets wound fluid, it undergoes a fascinating transformation, turning into a soft, conforming gel. This gel gently fills the entire wound cavity, leaving no empty space for bacteria to thrive. Because they come in both flat sheets and rope forms, they are perfect for packing deep or irregularly shaped wounds, turning a difficult situation into a manageable, healing environment.
This infographic shows just how much more effective an advanced dressing can be compared to traditional gauze.
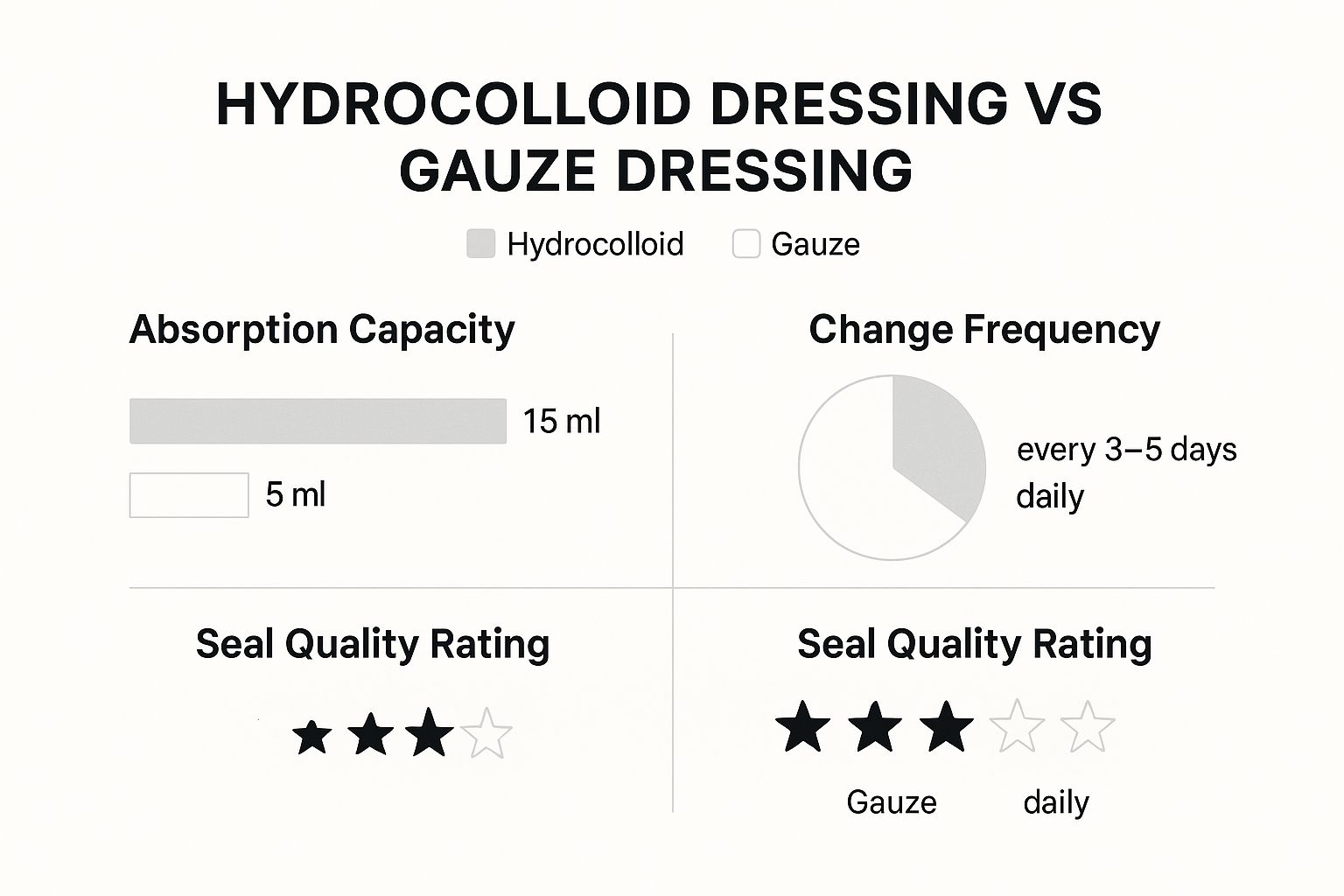
As you can see, the advanced dressing's ability to absorb more and create a better seal means it needs changing far less often. This leads to a more stable healing environment with fewer disruptions for the patient.
Tackling Infection with Antimicrobial Dressings
Sometimes, the single biggest barrier to healing is infection. For wounds that are already infected or are at a high risk of becoming so, an antimicrobial dressing is essential. These dressings are embedded with agents that actively kill microorganisms or stop them from multiplying in the wound bed.
Common antimicrobial agents include:
- Silver: A powerful, broad-spectrum agent that’s effective against a huge range of bacteria and fungi.
- Medical-Grade Honey: Creates an acidic environment that bacteria hate and also helps to gently clean the wound.
- Iodine (Cadexomer): This form releases iodine slowly for a sustained antimicrobial effect, making it especially useful for wounds with a lot of dead tissue (slough).
Choosing the right antimicrobial can be the deciding factor in getting a wound’s bacterial load under control, allowing the body’s own healing mechanisms to finally do their job. This is particularly vital for chronic wounds, which often get stuck in a non-healing state due to persistent, low-level infection.
To help you decide which dressing is right for your situation, here is a quick comparison table.
Selecting the Right Advanced Dressing
| Wound Characteristic | Foams | Alginates | Antimicrobials |
|---|---|---|---|
| Exudate Level | Moderate to Heavy | Heavy to Very Heavy | Varies (depends on base dressing) |
| Infection | No | No | Yes (infected or at-risk) |
| Wound Depth | Shallow | Deep, Tunneling | Shallow or Deep |
| Primary Goal | Absorb & Protect | Absorb & Fill | Reduce Bioburden |
This table provides a starting point, but always remember that a thorough clinical assessment is key to making the best choice for each individual wound.
Jump-Starting Healing with Bioactive Dressings
But what if a wound is clean and well-managed, yet it has simply stalled out? For these stubborn, non-healing chronic wounds, bioactive dressings can provide the nudge they need. Unlike other dressings that just manage the wound environment, bioactive materials get directly involved in the healing cascade.
Collagen dressings are a perfect example. Collagen is the main protein that gives our skin its structure. By placing a collagen dressing onto a wound, you’re essentially providing a scaffold for the body's own cells to crawl into and start rebuilding tissue. They are especially effective for chronic wounds like those found in patients with diabetes. Understanding the challenges of treating diabetic foot ulcers really highlights why these advanced interventions are so important.
Ultimately, these dressings represent a shift in thinking—from passively managing a wound to actively, biologically kick-starting the healing process.
A Framework for Selecting the Right Dressing

Knowing all the different types of wound dressings is one thing. The real art and science of wound care, though, lies in turning that product knowledge into a confident, effective decision right at the patient's side. It’s not about grabbing the newest or most expensive dressing off the shelf; it's about matching the product to the wound's specific, ever-changing needs.
To do this well, seasoned clinicians don't just guess. They use a structured approach to guide their thinking. One of the most practical and respected methods is the T.I.M.E. framework, a system that organizes wound assessment into four key areas. Think of it as your pre-flight checklist for wound care—it ensures you've covered all the critical factors before you even reach for a dressing.
Using the T.I.M.E. Framework for Assessment
The T.I.M.E. acronym is a simple but incredibly powerful tool for looking at a wound as a whole, making sure no important detail gets missed.
- T – Tissue: What does the wound bed actually look like? Is it healthy, pink, and bumpy with granulation tissue? Or are you seeing yellow slough or even black, leathery eschar (dead tissue)? The tissue type tells you whether you need a dressing that encourages new growth, helps clear out debris, or adds moisture to soften up that tough, non-viable tissue.
- I – Infection/Inflammation: Are there any tell-tale signs of infection—like spreading redness, warmth, increased pain, or a foul odor? If the answer is yes, you'll want to prioritize an antimicrobial dressing. If not, a standard, non-antimicrobial dressing is probably the better and more appropriate choice.
- M – Moisture: How much fluid, or exudate, is the wound producing? Is it sopping wet, just a little damp, or totally dry? This is a huge factor. It’s the difference between needing a super-absorbent dressing like an alginate for a heavily draining wound versus a moisture-donating hydrogel for a dry one.
- E – Edge: Take a close look at the wound's perimeter. Are the edges attached and slowly creeping inward, signaling healing? Or are they rolled, raised, or tunneled underneath? The condition of the wound edge is a story in itself, telling you if the wound is making progress or if your current plan needs a rethink.
The T.I.M.E. framework stops you from seeing a wound as just one problem. It forces you to see it as a dynamic environment and to ask the most important question: "What does this specific wound need right now to get to the next stage of healing?"
From Assessment to Application
Once you’ve run through your T.I.M.E. assessment, you can start connecting the dots to the right dressing. With a little practice, this thought process becomes second nature.
Let’s walk through a common scenario to see how this works in the real world.
Scenario: A patient presents with a diabetic foot ulcer on their heel.
- T (Tissue): The wound bed is about 70% covered in soft, yellowish slough.
- I (Infection): No obvious redness, warmth, or smell. Infection isn't the main worry at this moment.
- M (Moisture): The wound is producing a moderate amount of thick drainage.
- E (Edge): The edges are visible but don't seem to be advancing.
Based on this quick assessment, you need a dressing that can handle that moderate drainage while also helping the body break down and clear away the slough (a process called autolytic debridement). An alginate would likely be overkill and might dry the wound out too much. A simple gauze dressing would just stick and cause pain.
This is where a hydrocolloid or a foam dressing would be fantastic choices. Both are great at managing this level of moisture and will create the ideal environment to help soften and lift that slough.
Contrast that with a dry, necrotic wound, where a hydrogel would be the obvious choice to add moisture. The framework guides you to a logical solution every time. While this systematic approach is highly effective, it's worth noting that some older methods, like wet-to-dry wound care dressing changes, were used for debridement. Today, modern dressings often provide a more efficient and much less painful alternative.
Ultimately, a structured assessment like T.I.M.E. empowers you to make confident, evidence-based decisions. It shifts your focus from a confusing list of products to a clear, patient-centered plan, ensuring every wound gets exactly what it needs to heal.
The Future of Wound Care and Smart Dressings

Wound care is on the cusp of a significant transformation. We're moving beyond dressings that simply manage a wound's environment to creating ones that actively monitor it and adapt. The next generation of wound dressings will function less like a simple bandage and more like a sophisticated wearable health device, making the healing process faster, smarter, and incredibly personalized.
Think about a dressing that can alert you when it's time for a change or signal the very first signs of trouble before they’re visible to the naked eye. This isn't science fiction; it's the reality of smart dressings. These are not just passive materials. They have advanced sensors woven directly into the dressing itself.
These dressings can pick up on minute shifts within the wound bed—things like a change in pH or temperature, which are often the earliest tell-tale signs of an emerging infection. So, instead of waiting for redness, swelling, or pus, the dressing itself might change color, giving clinicians a crucial head start on intervention.
Customization and Targeted Delivery
The future is also about getting the fit just right, both in shape and in function. Researchers are hard at work developing 3D-printed dressings that can be created to match the exact size, shape, and even depth of a patient's wound. This precise fit eliminates the tiny gaps where bacteria love to multiply and ensures the entire wound bed is in contact with the dressing, creating an ideal healing environment.
But it doesn't stop with a custom fit. These advanced dressings will double as targeted delivery systems. Drug-eluting dressings are being engineered to release specific medications—like antibiotics, anti-inflammatories, or growth factors—directly into the wound. This approach concentrates the medicine exactly where it's needed most, reducing the risk of systemic side effects while maximizing the therapeutic impact.
The next frontier in wound management is not just about healing, but healing intelligently. By combining biosensors, custom manufacturing, and targeted drug delivery, future dressings will provide a level of personalized care that was once the stuff of science fiction, turning the dressing into an active partner in the recovery process.
Making Advanced Therapies More Accessible
This wave of innovation is also focused on bringing powerful treatments to more people. Take Negative Pressure Wound Therapy (NPWT), for instance. It's been a game-changer for complex wounds for years, but it has traditionally relied on bulky and expensive hospital equipment.
That’s all changing with the arrival of disposable, single-use NPWT systems. These lightweight, portable devices are making this gold-standard therapy practical for patients to use at home. This shift not only reduces the need for long hospital stays but also empowers people to heal comfortably in their own space. These advancements point to a clear future where every dressing is a precise, responsive tool designed for healing.
Common Questions About Wound Dressings
When you're dealing with wound care day in and day out, a lot of practical questions come up. Understanding the "why" behind what we do is just as important as the "how," especially when it comes to choosing the right dressing. Let's tackle some of the most common questions I hear from clinicians.
How Often Should a Wound Dressing Be Changed?
There's no magic number here. The old-school thinking of changing every dressing daily is long gone. The real answer depends entirely on the wound itself, the type of dressing you're using, and how much fluid (exudate) is coming out.
A good way to think about it is that the dressing tells you when it’s time for a change. A highly absorbent foam dressing might do its job for several days on a moderately draining wound. On the other hand, a simple gauze pad on a heavily weeping wound might need to be switched out much sooner. You change the dressing when it's saturated or no longer working, not just because the clock says so.
The golden rule for dressing changes is to follow the cues from the wound and the dressing. A change is needed when the dressing can no longer effectively manage the wound environment. This approach prevents unnecessary changes that can disturb the fragile, healing tissue.
Can You Combine Different Dressing Types?
Not only can you, but you absolutely should in many cases. Layering dressings is a smart and standard practice that allows you to tailor your treatment to a wound's specific needs. Think of it as using a primary dressing that touches the wound bed directly and a secondary dressing on top to secure it, protect it, or add an extra function.
Here are a couple of real-world examples:
- For a deep wound: You might use an alginate rope as the primary dressing to gently fill the cavity, then cover it with a secondary foam dressing to absorb any excess fluid and add a layer of protection.
- For a dry wound: You could apply a hydrogel (primary dressing) to add much-needed moisture, then place a transparent film over it (secondary dressing) to keep the gel in place and seal out contaminants.
What Is the Most Important Factor in Choosing a Dressing?
While features like absorbency and wear time are definitely part of the equation, the single most critical factor is a thorough and holistic wound assessment. A dressing is just a tool, and picking the right one is impossible without first understanding the job it needs to do.
You have to look at the whole picture: the patient's overall health, the wound's location, the amount of moisture, the type of tissue in the wound bed, and any signs of infection. A comprehensive assessment, like one using the T.I.M.E. framework, is what guides you to the right product. Your choice should always be driven by the wound’s needs, not just by what’s on the supply shelf.



