Effective wound healing is a cornerstone of patient recovery, and debridement is a critical first step. The process of removing dead, damaged, or infected tissue from a wound bed is essential for preventing infection, reducing inflammation, and stimulating the growth of healthy new tissue. Without proper debridement, even the most advanced wound dressings and therapies can fail, leaving patients with chronic, non-healing wounds that can significantly impact their quality of life.
However, not all debridement methods are created equal. The choice of technique depends on numerous factors, including the wound type, the amount of necrotic tissue, the patient's overall condition, and the clinical setting. Understanding the different types of wound debridement is vital for both healthcare professionals aiming to optimize care and for patients seeking to understand their treatment options.
This guide provides a comprehensive roundup of the six primary methods used in modern wound care. We will explore the specific indications, advantages, disadvantages, and practical scenarios for each technique, from the precision of surgical debridement to innovative biological therapies. Our goal is to offer a clear roadmap to selecting the most appropriate strategy for effective wound bed preparation and accelerating the healing process.
1. Sharp/Surgical Debridement
Sharp debridement is a highly precise and effective method for removing dead or nonviable tissue (necrotic tissue), foreign material, and biofilm from a wound. Often considered the gold standard among the different types of wound debridement, this technique is performed by a qualified healthcare professional using sterile instruments like scalpels, scissors, curettes, and forceps. The primary goal is to create a clean, healthy wound bed, which is essential for promoting healing.
This method can be performed in two distinct settings: conservatively at the patient's bedside or more aggressively in a sterile operating room environment. The choice depends on the wound's severity, size, and the patient's overall health status. By directly cutting away devitalized tissue, sharp/surgical debridement provides immediate results, making it the fastest way to prepare a wound for advanced therapies or closure.
When to Use Sharp/Surgical Debridement
This approach is indicated for wounds with a significant amount of necrotic tissue, such as thick, leathery eschar or moist, sloughy tissue. It is particularly crucial for advancing the healing of chronic wounds that have stalled.
- Diabetic Foot Ulcers: It is highly effective for removing calluses and necrotic tissue, which is a critical step in managing these complex wounds. For a deeper dive into this specific application, you can explore comprehensive strategies for treating diabetic foot ulcers.
- Pressure Ulcers (Bedsores): Essential for removing dead tissue in Stage III and IV pressure injuries to assess the full depth and facilitate granulation.
- Infected Wounds: When a wound is infected, rapid removal of the nonviable tissue that harbors bacteria is necessary to control the infection and prevent it from spreading.
- Surgical Wounds: Used to manage wounds that have dehisced (reopened) or become infected post-operation.
Key Considerations and Best Practices
While highly effective, sharp debridement requires skill, precision, and a controlled environment.
Key Insight: Proper patient preparation is non-negotiable. This includes managing the patient's pain with appropriate analgesia before the procedure begins and ensuring they are in a comfortable, stable position.
To ensure a successful and safe procedure, clinicians should:
- Ensure Adequate Visualization: Use proper lighting to clearly distinguish between viable and nonviable tissue.
- Maintain Sterility: A strict sterile or clean technique prevents introducing new bacteria into the wound.
- Manage Bleeding: Have hemostatic agents (e.g., silver nitrate, gelfoam) readily available to control any bleeding, which is a common occurrence.
This summary box highlights the essential components of sharp/surgical debridement, breaking down the tools, speed, and settings.
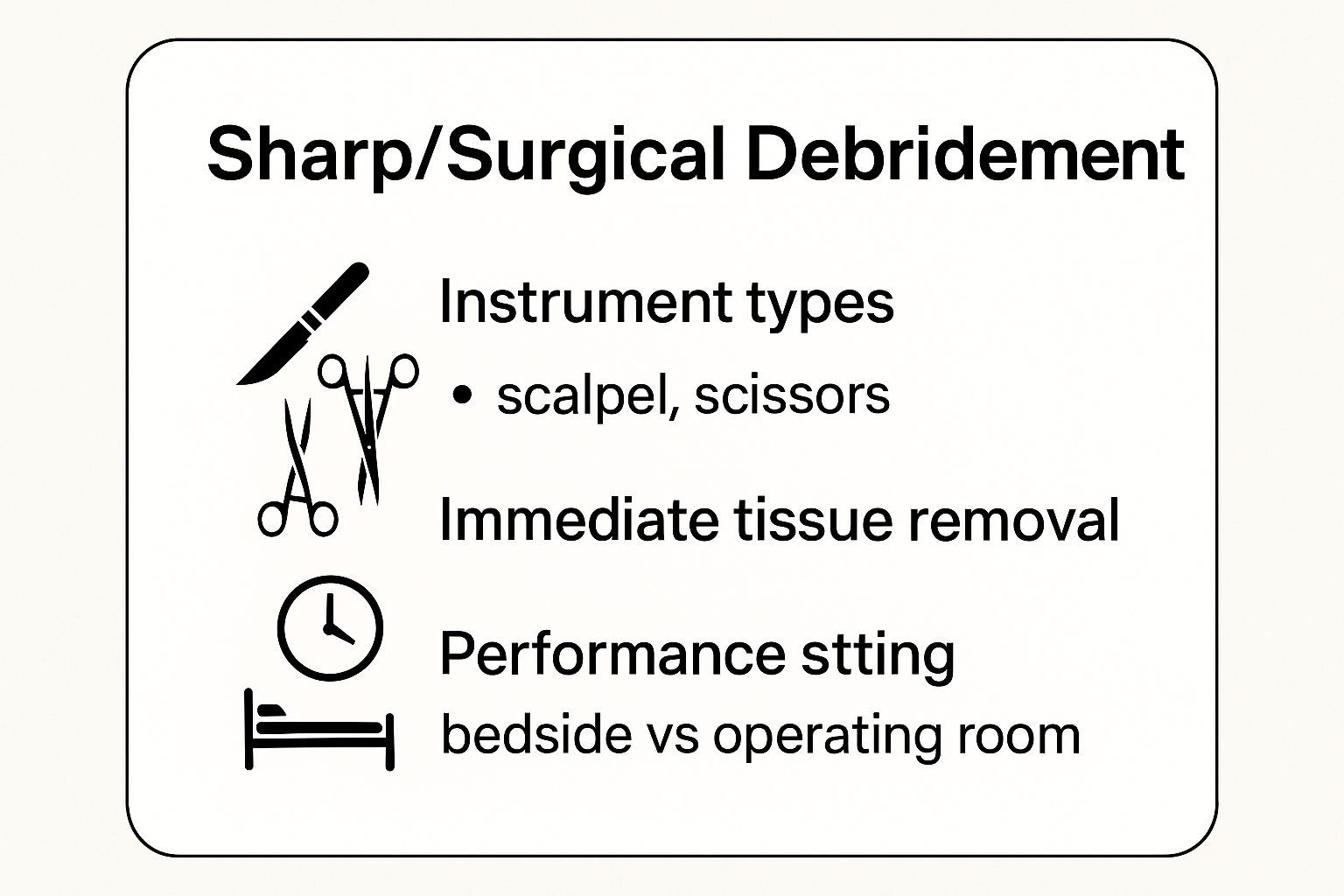
The infographic effectively illustrates that sharp debridement is a versatile procedure adaptable to both bedside and operating room settings, chosen for its unmatched speed in tissue removal. The following video demonstrates the meticulous nature of a sharp debridement procedure.
2. Enzymatic Debridement
Enzymatic debridement is a selective and less invasive method that uses naturally occurring proteolytic enzymes to liquefy and break down necrotic tissue. As one of the more targeted types of wound debridement, this approach involves applying a prescribed ointment or solution, such as collagenase, directly to the wound bed. These enzymes specifically target and dissolve devitalized tissue and slough while leaving healthy, viable tissue unharmed.
This biochemical process offers a gentler alternative to mechanical or sharp methods, making it ideal for patients who cannot tolerate more aggressive procedures. The enzymes work continuously between dressing changes, slowly but effectively cleaning the wound and preparing it for healing. It is a preferred method in settings where surgical intervention is not feasible or desired.

When to Use Enzymatic Debridement
This method is best suited for chronic wounds with moderate amounts of necrotic tissue, especially when the patient is not a candidate for surgery due to health status or pain sensitivity. It is also a valuable option for ongoing care in long-term facilities or home settings.
- Venous Leg Ulcers: Effective for removing fibrinous slough that commonly covers these wounds, promoting a clean base for compression therapy.
- Pressure Ulcers (Bedsores): Can be used on Stage III or IV pressure injuries to gently debride the wound, particularly in frail or elderly patients.
- Diabetic Foot Ulcers: A good choice for patients with poor circulation where sharp debridement might pose a higher risk of injury to surrounding tissue.
- Burns: Used in managing second and third-degree burns to selectively remove eschar without damaging the delicate, regenerating tissue underneath.
Key Considerations and Best Practices
Successful enzymatic debridement hinges on proper application and creating the right wound environment for the enzymes to work effectively.
Key Insight: The efficacy of enzymatic debridement is highly dependent on a moist wound environment. A dry wound bed will deactivate the enzymes, rendering the treatment ineffective.
To maximize the benefits of this method, clinicians and caregivers should:
- Apply a Thin Layer: The ointment should be applied directly and only to the necrotic tissue, typically about the thickness of a nickel.
- Protect Periwound Skin: Use a moisture barrier cream or skin sealant on the healthy skin surrounding the wound to prevent maceration or irritation.
- Choose the Right Dressing: Cover the wound with a moisture-retentive secondary dressing to keep the wound bed moist and the enzymes active.
- Monitor for Reactions: While rare, be vigilant for signs of local irritation or allergic reaction and discontinue use if they occur. For those managing wounds outside a clinical setting, understanding these nuances is critical. You can explore more about this topic in our guide to at-home wound care.
3. Autolytic Debridement
Autolytic debridement leverages the body's own innate healing processes to liquefy and separate necrotic tissue from the healthy wound bed. It is one of the most selective and least invasive types of wound debridement, working by creating a moist, warm environment that encourages the body's own enzymes, such as proteases and collagenases, to break down dead tissue. This process is facilitated by applying moisture-retentive dressings that trap wound fluid against the necrotic material.
This method is gentle, virtually painless for the patient, and requires minimal clinical skill to apply the dressing. However, it is the slowest form of debridement and requires patience, as the natural process can take days or weeks. It is an excellent choice for patients who cannot tolerate more aggressive methods or for those receiving palliative or home care.
When to Use Autolytic Debridement
This approach is best suited for non-infected wounds with a small to moderate amount of slough or eschar. It is ideal for patients where comfort and pain management are priorities.
- Pressure Ulcers (Bedsores): Especially effective for Stage II or III pressure injuries with minimal necrotic burden, particularly in hospice or home care settings. To learn more about managing these wounds at home, explore these detailed guidelines for pressure ulcer treatment and home care.
- Chronic Venous Leg Ulcers: A common choice for removing soft slough from venous ulcers, as long as there is no active infection and circulation is adequate.
- Diabetic Ulcers: Can be used on diabetic foot ulcers with small amounts of nonviable tissue, provided there is no sign of critical limb ischemia or infection.
- Pediatric Wounds: The painless nature of autolytic debridement makes it an excellent option for children, minimizing distress during dressing changes.
Key Considerations and Best Practices
Success with autolytic debridement hinges on maintaining a perfect moisture balance without harming the surrounding skin.
Key Insight: The cornerstone of autolytic debridement is selecting the right moisture-retentive dressing. Hydrocolloids, hydrogels, transparent films, and alginates are all effective, but the choice must be tailored to the wound’s exudate level.
To optimize the autolytic process, clinicians and caregivers should:
- Protect Periwound Skin: Apply a skin barrier or protectant to the healthy skin around the wound to prevent maceration (softening and breakdown due to excessive moisture).
- Monitor for Infection: Since this method creates a warm, moist environment, it's crucial to regularly monitor for signs of infection such as increased redness, pain, warmth, or purulent drainage. Autolytic debridement is contraindicated for infected wounds.
- Adjust Dressing Change Frequency: Dressings should be changed based on the amount of exudate. A saturated dressing should be changed promptly to prevent leakage and maceration, while changing a dry dressing too often can disrupt the healing environment.
4. Mechanical Debridement
Mechanical debridement involves the physical removal of dead tissue and contaminants from a wound surface using mechanical force. Unlike more selective methods, this approach uses friction, irrigation, or adhesion to lift away slough, eschar, and other debris. Among the various types of wound debridement, it is often considered a non-selective method, as it can sometimes remove healthy granulation tissue along with the nonviable material.
The techniques can range from simple dressing applications to more advanced hydrotherapy. The primary goal is to physically dislodge and clear the wound bed, disrupting biofilm and preparing the surface for healing. The choice of technique depends on the wound type, the amount of necrotic tissue, the patient's tolerance, and the clinical setting.
When to Use Mechanical Debridement
This method is most appropriate for wounds with moderate amounts of necrotic debris or slough that is loosely adherent. It can be an effective initial step to clean a wound before transitioning to more selective debridement techniques.
- Chronic Wounds with Slough: Pulsatile lavage can effectively cleanse chronic ulcers by using pressurized, sterile fluid to flush away dead tissue and bacteria.
- Contaminated Traumatic Wounds: High-pressure irrigation is a classic use case, helping to remove dirt, gravel, and other foreign bodies from acute injuries to reduce the risk of infection.
- Burn Wounds: Whirlpool therapy, although used less frequently now due to cross-contamination risks, can help soften and remove necrotic tissue from large surface area burns.
- Wounds with Loosely Adherent Debris: Wet-to-dry dressings are a common, though older, method. A moist gauze is applied to the wound, allowed to dry, and then removed, pulling away debris with it. To better understand this specific technique, you can read about the process of wet-to-dry wound care dressing changes.
Key Considerations and Best Practices
Because mechanical debridement is non-selective, careful application is crucial to avoid damaging healthy tissue and causing unnecessary pain.
Key Insight: Patient comfort is paramount. Mechanical methods, especially scrubbing or certain dressing removals, can be painful. Pre-medicating with appropriate analgesics before the procedure is an essential best practice.
To perform mechanical debridement safely and effectively, clinicians should:
- Use Appropriate Pressure: When irrigating, use a pressure that is sufficient to cleanse the wound without driving bacteria deeper into the tissue.
- Avoid Aggressive Scrubbing: Gentle scrubbing is sometimes needed, but aggressive action can traumatize the wound bed and impede healing.
- Monitor the Wound Response: Closely observe the wound for signs of trauma, such as pinpoint bleeding (petechiae) or damage to new granulation tissue, and adjust the technique accordingly.
- Choose Sterile Solutions: Always use sterile solutions like normal saline for irrigation to prevent introducing new pathogens into the wound.
5. Biological Debridement (Maggot Therapy)
Biological debridement, more widely known as maggot therapy, is a fascinating and highly selective method that uses sterile, medical-grade larvae of the green bottle fly (Lucilia sericata) to clean wounds. This approach, though ancient in origin, is an FDA-approved modern treatment and a powerful option among the various types of wound debridement. The larvae are applied directly to the wound, where they work by consuming necrotic tissue, dead cells, and harmful bacteria while leaving healthy, viable tissue completely unharmed.
The larvae secrete enzymes that liquefy dead tissue, making it easy for them to ingest. This process not only debrides the wound but also disinfects it by killing bacteria and stimulating the growth of healthy granulation tissue. Pioneered in its modern form by figures like Dr. Ronald Sherman and supplied by companies like BioMonde and Monarch Labs, maggot therapy offers a unique, natural solution for complex wounds.

When to Use Biological Debridement
This method is exceptionally useful for non-healing wounds where surgical debridement is not an option, or for wounds with antibiotic-resistant bacteria like MRSA. It is particularly effective for removing slough and soft necrotic tissue.
- Diabetic Foot Ulcers: An excellent choice for managing wounds infected with resistant bacteria or in patients who are poor surgical candidates.
- Chronic Venous Leg Ulcers: Helps break down stubborn slough and biofilm, promoting a healthier wound bed and preparing it for healing.
- Pressure Ulcers (Bedsores): Effective for debriding wounds in patients with spinal cord injuries or limited mobility where surgical risk is high.
- Post-Surgical and Traumatic Wounds: Can be used to clean non-healing surgical sites or traumatic wounds that have a significant amount of necrotic tissue.
Key Considerations and Best Practices
Successful maggot therapy requires careful planning, patient education, and specific application techniques to maximize its benefits and ensure patient comfort.
Key Insight: Patient acceptance is paramount. Thoroughly explaining the procedure, its benefits, and what to expect can alleviate anxiety and secure informed consent, which is a critical first step.
To ensure a safe and effective treatment cycle, clinicians should:
- Use Proper Containment: The larvae must be contained within the wound bed using a special "cage-like" dressing that allows air to circulate but prevents them from escaping.
- Monitor the Patient: Check for any rare allergic reactions to larval secretions and manage any "tickling" or crawling sensations the patient might feel.
- Adhere to Timelines: The larvae are typically left in the wound for 48 to 72 hours before being removed. Adhering to these intervals is crucial for effectiveness and safety.
6. Ultrasonic Debridement
Ultrasonic debridement is an advanced, selective method that uses high-frequency sound waves (ultrasound) to precisely remove nonviable tissue, slough, and biofilm. This technology, recognized as one of the more modern types of wound debridement, works by generating cavitation and microstreaming effects through a saline solution. The sound waves create tiny, oscillating bubbles that gently lift and separate dead tissue and bacteria from the wound bed while preserving healthy, viable tissue.
This technique, often performed with devices like the Misonix SonicOne or Söring systems, combines the precision of a controlled instrument with a gentle, tissue-sparing action. It is highly effective at disrupting biofilm, a major barrier to healing in chronic wounds, and stimulating the wound bed to promote the formation of healthy granulation tissue. The process effectively cleans the wound on a microscopic level.
When to Use Ultrasonic Debridement
This method is ideal for wounds where precision is key and minimizing damage to surrounding healthy tissue is a priority. It is particularly effective for removing adherent slough and biofilm that other methods might miss.
- Chronic Diabetic Foot Ulcers: Excellent for clearing biofilm and slough, which are common culprits in stalled diabetic ulcers.
- Venous Leg Ulcers: Effectively removes fibrinous slough that is often tightly adhered to the wound bed in these types of wounds.
- Pressure Ulcers (Bedsores): Useful for cleaning wounds with complex shapes or undermining, as the ultrasonic energy can reach areas that are difficult to access with mechanical instruments.
- Post-Surgical Wound Complications: Helps manage infected or dehisced surgical sites by thoroughly cleaning the wound bed to prepare it for closure or advanced therapies.
Key Considerations and Best Practices
Successful ultrasonic debridement requires specialized equipment and training to ensure both safety and efficacy.
Key Insight: The success of ultrasonic debridement hinges on maintaining constant contact between the probe and the wound bed through a liquid medium, typically sterile saline. This "coupling" is essential for the transmission of ultrasonic energy to the target tissue.
To optimize outcomes, healthcare providers should:
- Use Appropriate Settings: Adjust the frequency and power settings on the device based on the type and amount of necrotic tissue present.
- Manage Aerosolization: The process can create a mist of saline and microscopic debris, so using appropriate personal protective equipment (PPE) and containment systems is crucial to protect both the clinician and the patient.
- Combine with Other Therapies: After debridement, selecting an appropriate dressing is critical to maintain a moist environment and support the healing process. For more information on wound care strategies, you can explore insights on how to heal deep wounds faster.
6 Types of Wound Debridement Comparison
| Debridement Type | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Sharp/Surgical Debridement | High – requires skilled practitioner & possible anesthesia | Sterile surgical instruments, clinical setting | Immediate, precise removal of necrotic tissue | Thick eschar on diabetic foot ulcers, burn wounds, surgical site infections | Fastest, highly selective, cost-effective, reduces bacterial load |
| Enzymatic Debridement | Moderate – topical enzyme application with multiple uses | Enzyme preparations (collagenase, papain-urea) | Selective necrotic tissue breakdown, slower onset | Chronic ulcers, infected wounds, patients intolerant of sharp methods | Painless, selective, can be used on infected wounds, continuous action |
| Autolytic Debridement | Low – passive with moisture-retentive dressings | Hydrogels, hydrocolloids, foam dressings | Slow natural debridement via body's enzymes | Minimal necrosis, pain-sensitive patients, hospice care | Completely painless, cost-effective, promotes natural healing |
| Mechanical Debridement | Moderate – physical removal, technique sensitive | Basic supplies like wet-to-dry dressings, irrigation tools | Immediate removal but non-selective tissue damage possible | Loose necrotic tissue, burn patients, traumatic wounds | Low cost, readily available, immediate feedback |
| Biological Debridement (Maggot Therapy) | Moderate to high – requires specialized handling & patient acceptance | Sterile fly larvae and containment dressings | Selective necrotic tissue removal with antimicrobial effect | Infected diabetic ulcers, antibiotic-resistant wounds | Highly selective, antimicrobial, stimulates healing |
| Ultrasonic Debridement | High – specialized ultrasonic equipment and training | Ultrasonic devices, sterile saline coupling | Selective necrotic and biofilm removal, minimal pain | Complex wounds with biofilm, irregular geometry | Precise, preserves healthy tissue, effective biofilm disruption |
Choosing the Right Path to Wound Recovery
Navigating the diverse landscape of wound care reveals that the various types of wound debridement are not competing options, but rather specialized tools in a clinician's toolkit. The journey from a non-healing wound to healthy, granulated tissue is rarely a straight line. It requires a nuanced understanding that the "best" method is always the one most appropriate for the specific wound, the individual patient, and the clinical setting.
This article has detailed six distinct approaches, from the rapid precision of surgical debridement to the gentle, natural process of autolytic debridement. We've explored how enzymatic ointments can selectively target non-viable tissue and how biosurgery, using medical-grade maggots, offers a unique solution for complex wounds. Each method carries its own set of indications, benefits, and considerations, underscoring the importance of a comprehensive initial assessment.
Key Takeaways for Effective Wound Management
The central theme connecting all effective debridement strategies is the principle of individualized care. A successful outcome hinges on matching the debridement technique to the specific clinical picture.
- Wound Characteristics are Paramount: The type and amount of necrotic tissue (eschar vs. slough), presence of infection, wound location, and depth are primary factors guiding the decision.
- Patient-Centric Approach: A patient's overall health, pain tolerance, comorbidities (like diabetes or vascular disease), and access to care are just as crucial as the wound's condition.
- Dynamic Treatment Plans: Wound care is not static. A wound may initially require aggressive sharp debridement to remove a large area of dead tissue, followed by enzymatic or autolytic methods to maintain a clean wound bed as it heals. The treatment plan must be flexible and responsive to the wound's progress.
Actionable Next Steps for Patients and Providers
Understanding the different types of wound debridement empowers both patients and healthcare providers to engage in more meaningful conversations about care plans. If you are a patient or caregiver, use this knowledge to ask informed questions about why a particular method is being recommended. If you are a clinician, continually reassessing the wound at each visit ensures the chosen debridement strategy remains optimal.
Mastering these concepts is not just an academic exercise; it has a profound impact on real-world outcomes. The right debridement choice can accelerate healing, reduce the risk of severe infections like sepsis or osteomyelitis, minimize pain, and ultimately improve a patient's quality of life. It is the foundational step upon which all other advanced wound therapies are built. A clean, prepared wound bed is essential for healing to begin in earnest.
Is a non-healing wound causing you or a loved one distress? Rapid Wound Care specializes in bringing expert wound assessment and advanced debridement services directly to your home or care facility. Our skilled clinicians determine the most effective type of debridement for your specific situation, ensuring personalized and convenient care that promotes faster healing. Visit Rapid Wound Care to learn how our at-home services can start you on the right path to recovery today.

