Your Body's Hidden Superpower: The Healing Orchestra
Imagine slicing your finger while chopping vegetables. Ouch! In that instant, a hidden team of microscopic specialists springs into action, initiating a complex four-stage process known as wound healing. It’s a finely tuned system, perfected over generations, designed to efficiently address the injury and restore your body to its normal state. Understanding these stages can empower you to actively participate in your own recovery.
The first phase, hemostasis, is the emergency response team. Think of it like paramedics arriving at the scene of an accident. Their first priority is to stop the bleeding. Similarly, your body constricts blood vessels and initiates the clotting cascade, creating a protective plug to seal the wound. This vital first step sets the stage for the entire healing journey.
Next up is inflammation, the cleanup crew. While inflammation often brings discomfort – redness, swelling, and tenderness – it's essential for clearing out debris and battling potential infection. Picture them as a dedicated sanitation team diligently preparing the construction site for rebuilding. These signs, while sometimes unpleasant, are a clear indication that this crucial phase is underway.
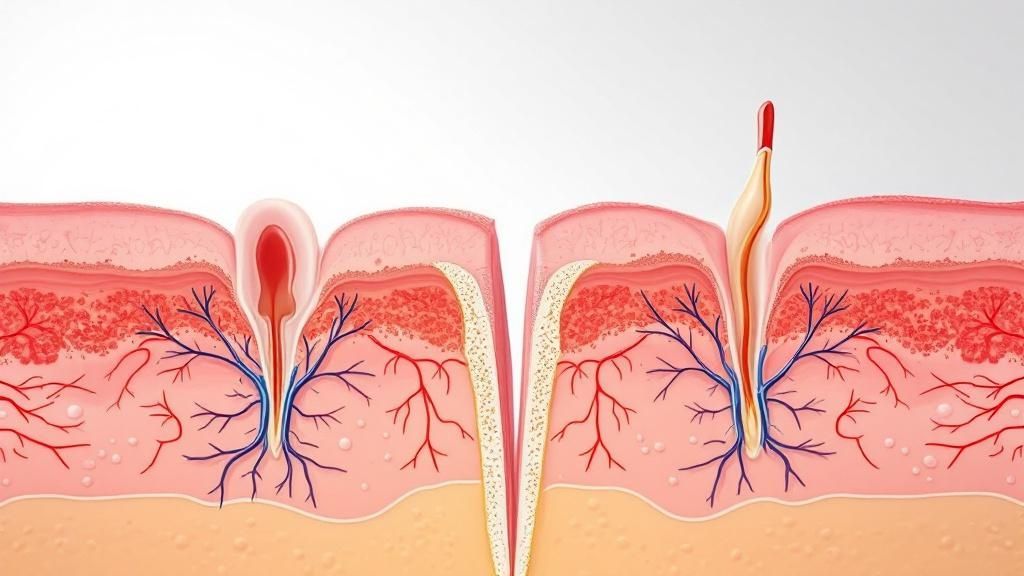
This illustration visualizes the typical phases of wound healing:
The diagram highlights how the healing stages overlap, emphasizing how each phase lays the groundwork for the next. For a deeper dive into different wound types, you might find this helpful: learning more about different wound types.
Once the cleanup is complete, proliferation begins – the construction phase. This is where the real rebuilding happens. Cells multiply rapidly, laying down collagen, a protein that forms the structural framework of new skin, like the scaffolding of a building. New blood vessels also sprout, delivering vital oxygen and nutrients to the growing tissue. This phase showcases your body's impressive regenerative capabilities.
Finally, we have remodeling, the finishing crew. This long-term refinement process can continue for months or even years. Think of it like the detailed work of painters and interior designers perfecting the final touches. The new tissue gradually gains strength and flexibility, and the scar fades. This final act demonstrates your body’s commitment not just to patching you up, but to restoring the injured area as closely as possible to its original condition. Understanding these four stages empowers you to become an active participant in your own healing journey.
Act One: Hemostasis – Your Body's Emergency Response Team
Imagine your body is like a bustling city. Suddenly, there's an emergency – a burst pipe! That's similar to what happens when you get injured. Your body’s first responders, the hemostasis team, immediately rush to the scene to stop the "flood" – the bleeding. This first phase of wound healing is all about damage control.
This initial response is critical to prevent significant blood loss and protect the wound from infection. Think of your blood vessels as the city's intricate network of roads. In an emergency, traffic has to be redirected, and your body does this through vasoconstriction. The blood vessels near the injury constrict, reducing blood flow and minimizing blood loss.
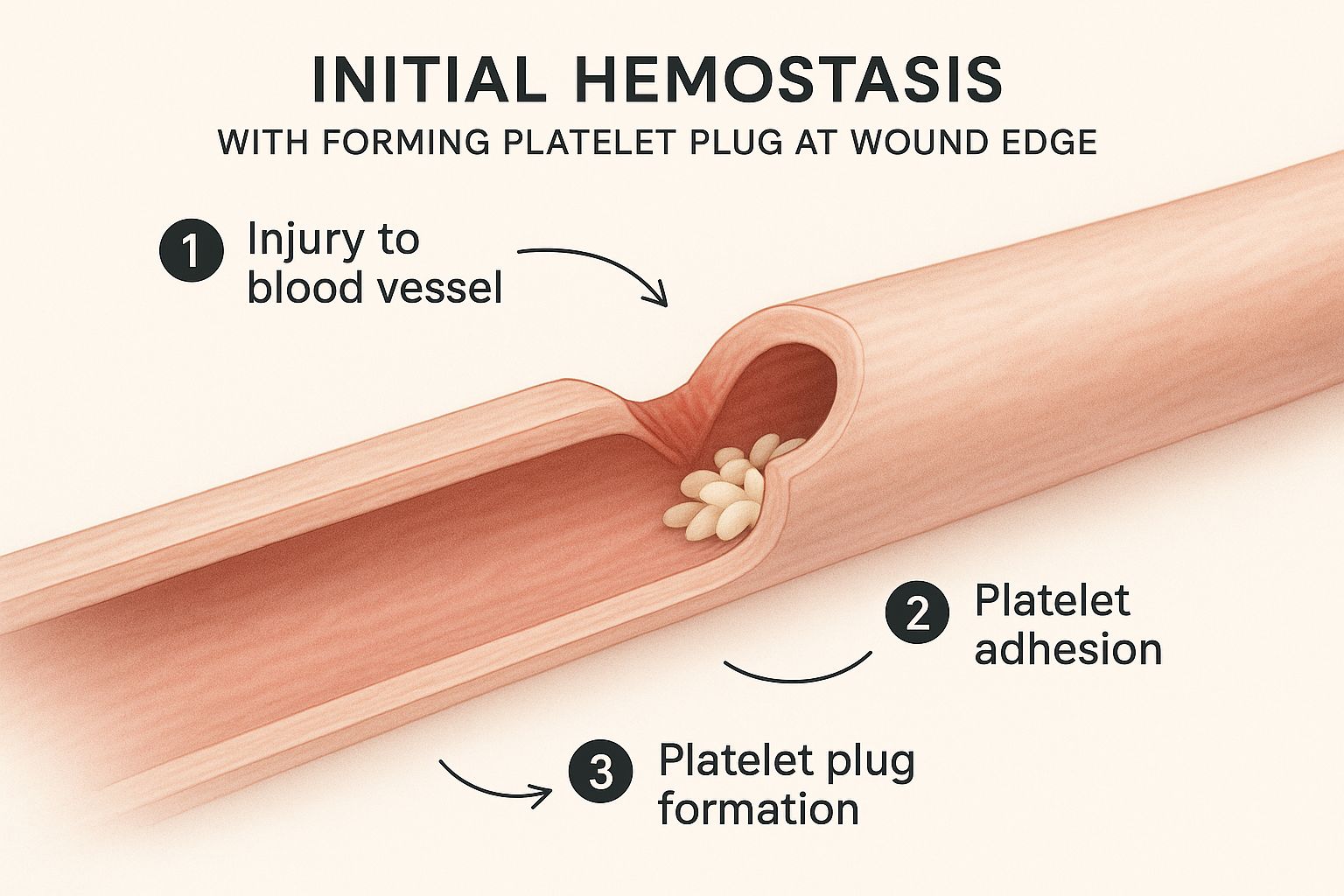
This image visualizes that first step in hemostasis. See how the platelets, tiny cell fragments in your blood, gather at the injury site? They become sticky and clump together, forming a plug to seal the breach, much like a temporary patch on that burst pipe. This plug is the first line of defense against further bleeding.
At the same time, a more permanent solution is underway – the coagulation cascade. Think of it as a construction crew arriving to lay down a strong foundation. Various clotting factors work together to create a fibrin mesh, a net-like structure that traps blood cells and reinforces the platelet plug. This forms the stable scab, your body's natural bandage.
To help visualize the timeline of this rapid response, take a look at the table below:
Hemostasis Timeline and Key Events
This table provides a detailed breakdown of what happens during the hemostasis phase, from the initial injury to the formation of a stable clot.
| Time Frame | Biological Process | Visible Signs | Care Considerations |
|---|---|---|---|
| Seconds to Minutes | Vasoconstriction | Bleeding slows | Applying direct pressure can assist this natural process |
| Minutes | Platelet Plug Formation | Blood starts to clot, a soft, jelly-like plug may be visible | Avoid disturbing the forming clot |
| Minutes to Hours | Coagulation Cascade | Clot becomes firmer, a scab begins to form | Keep the wound clean and protected |
As you can see, hemostasis is a rapid and highly effective process. The quick action of vasoconstriction, platelet plug formation, and the coagulation cascade stops bleeding and forms a protective scab, setting the stage for the next phase of healing. Chronic wounds, those that fail to heal within four to six weeks, affect over 6.5 million people in the United States alone, highlighting the importance of understanding these initial stages. For more in-depth information, you can explore this resource: Learn more about wound healing stages.
This image from Johns Hopkins Medicine emphasizes how each phase of wound healing builds upon the previous one. Hemostasis, the initial clotting and sealing of the wound, lays the groundwork for the subsequent repair and regeneration. This precisely orchestrated process is crucial for effective healing. With the "emergency" contained, the body can now shift its focus to the next act: inflammation.
Act Two: Inflammation – The Cleanup Crew Takes Charge
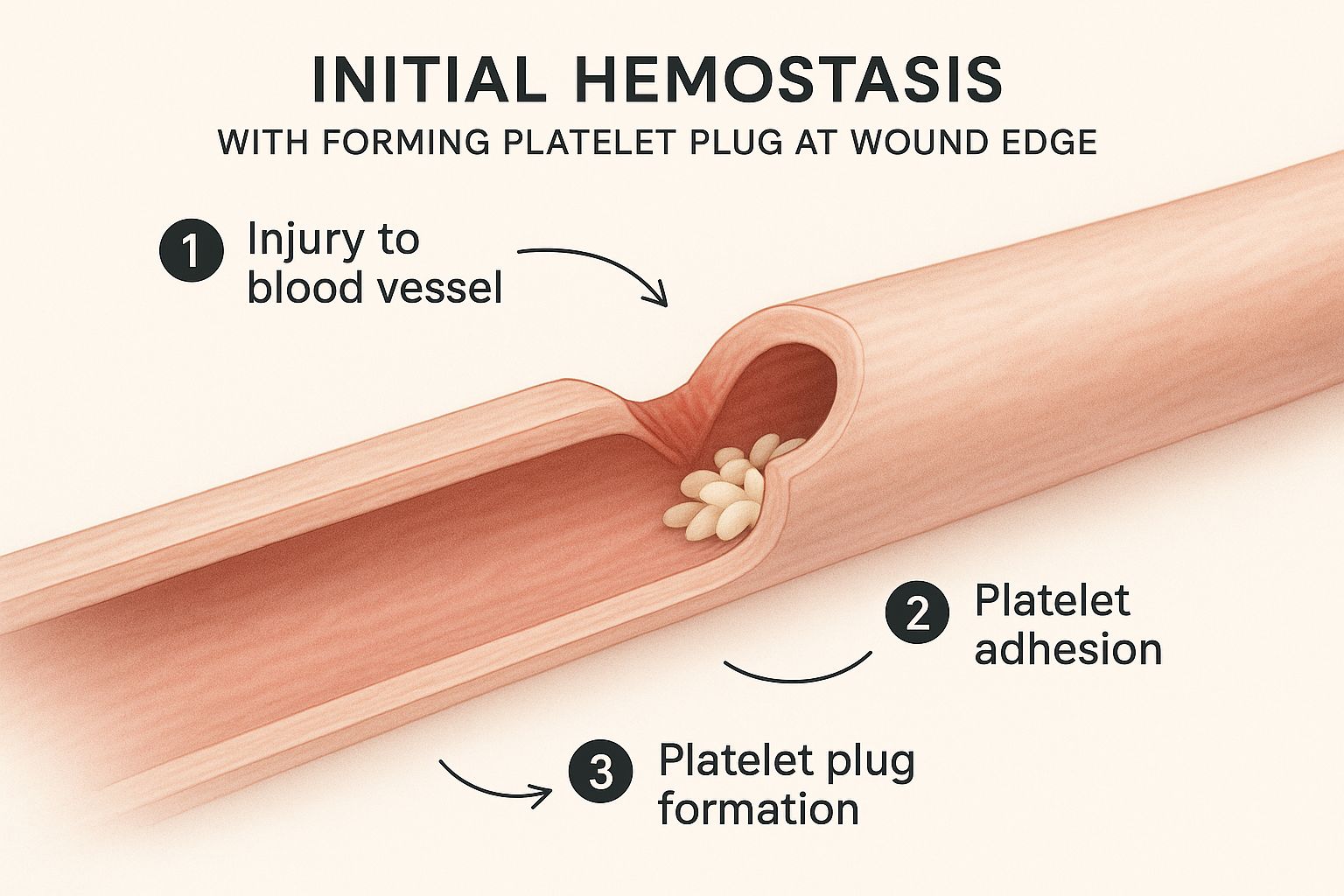
After the initial "stop the bleeding" action of hemostasis, the next act in wound healing is inflammation. While we often think of inflammation as a bad thing, it's actually a vital part of healing. Imagine it as your body sending in a specialized cleanup crew to the injury site.
This cleanup crew consists of different cells, primarily white blood cells. These cells rush to the wound to clear out any debris and fight off potential infection. This is why the wound might become red, swollen, and tender. These aren't signs that something's wrong; they're signs that your immune system is doing its job.
This illustration shows the inflammation stage in action. You can see the influx of white blood cells and other immune cells into the wound area, a visual representation of your body's active response to the injury. This coordinated effort preps the wound for the next stage of healing.
Inflammation is crucial for clearing the wound and making way for new tissue growth. This phase typically lasts up to seven days in acute wounds, but it can be longer in chronic wounds. Infections during this phase can significantly delay healing. In the United States, wound infections account for roughly 20% of all hospital-acquired infections. This highlights the importance of proper wound care during this crucial period. Learn more about this at wound healing stages and infections.
Setting the Stage for Repair
The inflammation stage also sets the scene for the next phase of healing: proliferation. During inflammation, specialized cells release growth factors. These growth factors act like messengers, telling the body to start rebuilding the damaged area. Think of them as the foremen on a construction site, directing the work that needs to be done. For more information on wound care during this stage, check out our guide on wet-to-dry wound care dressing changes. While inflammation might be uncomfortable, it's a necessary step that allows your body to move on to the rebuilding phase.
Act Three: Proliferation – The Master Builders Get to Work
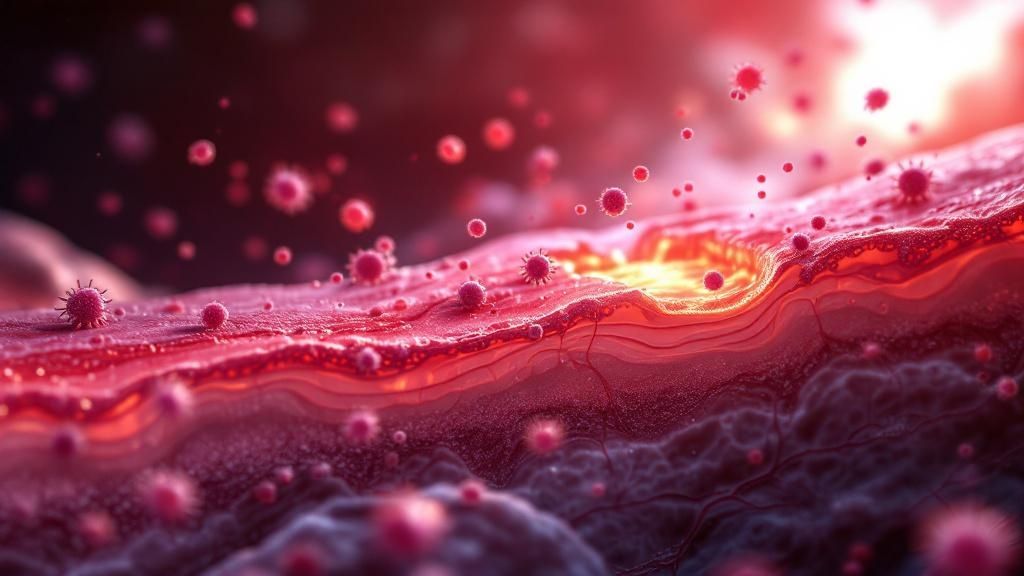
After the inflammation phase’s cleanup crew has finished, the true reconstruction begins. This third stage, proliferation, is a hive of activity, much like a bustling construction site. Specialized cells, acting as tiny architects and builders, work tirelessly to rebuild the damaged tissue.
One of the most fascinating processes during proliferation is angiogenesis: the creation of new blood vessels. Picture these new vessels as freshly paved highways, transporting vital nutrients and oxygen to the construction site. This delivery service is crucial for fueling the energy-intensive work of tissue regeneration.
This image provides a glimpse into the intricate network of new blood vessels that form during proliferation. These vessels are the lifeline of the repair process, delivering the essential building blocks for tissue growth and repair. It's a powerful visual reminder of our body's remarkable ability to rebuild itself.
Another key player is collagen, a tough, fibrous protein that acts like scaffolding for new tissue. Cells called fibroblasts produce collagen, laying down a framework that fills the wound and provides structural support. Think of this framework as the beams and supports of a building, giving the new tissue a strong foundation to grow on. For more tips on healing, check out this resource: learning how to heal deep wounds faster.
Building a Bridge of New Skin
As the wound fills with this new tissue, epithelialization begins. Cells from the wound edges migrate across the surface, like a bridge being constructed to close a gap. This fresh layer of skin is initially delicate, but it gradually toughens over time, restoring the skin’s protective barrier. This entire proliferation phase typically lasts from a few days to several weeks, varying depending on the wound’s size and depth.
To better understand the complexities of this phase, let's look at the following table:
Proliferation Phase: Key Processes and Outcomes
Comparison of the major biological processes occurring during tissue proliferation and their clinical significance
| Process | Duration | Key Cells Involved | Clinical Signs | Factors That Help |
|---|---|---|---|---|
| Angiogenesis | Several days to weeks | Endothelial cells | Redness, warmth around the wound | Oxygen, nutrients, growth factors |
| Collagen Synthesis | Several days to weeks | Fibroblasts | Increased wound strength, firmness | Protein-rich diet, Vitamin C |
| Epithelialization | Several days to weeks | Epithelial cells | Formation of new skin layer, wound closure | Moist wound environment, adequate hydration |
| Granulation Tissue Formation | Several days to weeks | Fibroblasts, inflammatory cells, new blood vessels | Pink, granular tissue filling the wound | Clean wound bed, adequate blood supply |
This table summarizes the key processes, their timelines, the cells involved, and what you might see happening with the wound during proliferation. Proper nutrition, especially a diet rich in protein and Vitamin C, is essential during this stage, providing the raw materials for new tissue construction.
The proliferation phase is a crucial step, laying the groundwork for wound closure. The global wound care market is projected to exceed $24 billion by 2025, highlighting the growing need for effective wound management. Learn more about wound healing from resources like Johns Hopkins Medicine. This incredible construction phase sets the stage for the final act of wound healing: remodeling.
Act Four: Remodeling – The Fine Art of Perfection
Welcome to the final act of wound healing: remodeling. Think of it less like a swift curtain drop, and more like a sculptor slowly revealing a masterpiece. This phase is a long-term commitment, refining and perfecting the repair work already done.
This meticulous process focuses on collagen reorganization. Initially, collagen fibers are laid down quickly, a bit like a hastily constructed scaffold. But during remodeling, these fibers are realigned and cross-linked, building a stronger, more organized structure. Imagine replacing a temporary wooden bridge with a sturdy, permanent steel one. This transformation can take months, even years, depending on the wound’s depth and size.
This diagram from the National Center for Biotechnology Information (NCBI) beautifully illustrates the overlapping phases of wound healing. Remodeling, the final stage, features ongoing collagen synthesis and degradation. It’s a continuous cycle of building up and breaking down, ultimately creating a stronger, more functional scar. The image really highlights the extended nature of this critical last phase.
The Story of Scars
Remodeling is where scars truly take shape. Ever wondered why some scars are prominent and raised, while others fade into near invisibility? Several factors contribute, including genetics, age, and the specifics of the original injury. Some people are predisposed to keloids – raised scars that extend beyond the original wound boundaries. Others might develop hypertrophic scars, which are raised but remain within the original wound area.
Supporting the Final Act
Even though remodeling is a long-term process, you can actively support it. Regular massage can improve tissue flexibility and minimize scar tissue buildup. Think of it like keeping the gears turning smoothly. Maintaining a healthy lifestyle, with good nutrition, sufficient sleep, and effective stress management, also plays a significant role. These practices are like providing the sculptor with the best tools and a calm, supportive studio to finish their masterpiece.
This final stage, often unseen, is a powerful testament to your body's incredible ability to repair and regenerate. It's a reminder that healing continues long after a wound appears closed, working diligently beneath the surface to restore strength and resilience.
When the Healing Story Goes Off Script
Sometimes, our bodies’ amazing healing abilities hit a snag. This section helps you spot when normal healing variations become complications that need attention. Think of it like a road trip: you expect a few bumps, but you need to know when to pull over for repairs. We’ll explore those subtle warning signs, from circulation issues that slow down the initial bleeding control to immune responses that turn helpful inflammation into a chronic problem.
Recognizing Roadblocks in Hemostasis
The first stage of healing, hemostasis, is all about stopping the bleeding. Imagine it like plugging a leak. But underlying conditions can throw a wrench in the works. People with poor circulation, like those with peripheral artery disease (PAD) where arteries become narrowed, might experience delayed clotting. Think of it like a kinked garden hose – it takes longer for the water (blood) to stop flowing. Certain medications, such as anticoagulants, can also thin the blood and extend bleeding time.
Inflammation: From Helper to Hindrance
Inflammation is crucial for healing, like a clean-up crew after demolition. But sometimes this helpful process goes overboard. If the inflammatory response lingers too long or becomes excessive, it turns into chronic inflammation. This is like the clean-up crew continuing to demolish perfectly good parts of the house. This persistent inflammation can damage healthy tissue and prevent the wound from moving on to the next repair phase. Autoimmune disorders, for example, can cause the immune system to overreact, leading to too much inflammation in the wound.
Proliferation Problems: Stalled Construction
The proliferation phase is where new tissue is built, like the reconstruction phase after demolition. But sometimes, construction stalls. Infection, like unwanted pests invading the construction site, can disrupt the delicate process of tissue regeneration. Signs of infection include increased pain, swelling, redness, and pus. Another potential problem is poor blood supply. If the wound doesn't get enough oxygen and nutrients, it's like the construction crew running out of materials – new tissue growth will be slow or even stop completely.
Remodeling Roadblocks: Imperfect Finishes
The final stage, remodeling, is like adding the finishing touches to the repaired house. But even here, problems can arise. Sometimes, the body overproduces collagen, leading to thick, raised scars called hypertrophic scars or keloids. Think of it as using too much spackle – it gets the job done, but the finish isn't smooth. Another issue is wound dehiscence, where the wound edges separate, like a poorly stitched seam coming undone. This is especially common in surgical wounds and can be caused by factors like infection, strain, or poor nutrition.
For helpful tips on wound care after leaving the hospital, check out this resource: Effective Post-Discharge Wound Care At Home. Recognizing these potential complications empowers you to seek timely medical attention. Understanding the stages of wound healing and what can go wrong allows you to be an active participant in your recovery. It’s not about worrying, it's about being informed and proactive in your healing journey.
Your Personal Healing Optimization Toolkit
Now that we understand the different stages of wound healing, let's talk about how you can actively support your body's natural repair process at home. Think of this as your personalized toolkit, filled with practical strategies to optimize your recovery.
Nutrition: Fueling the Repair Crew
Imagine your body is a construction site, busy rebuilding damaged tissue. Just like any construction crew, your body needs the right materials. In the early stages of healing, hemostasis (stopping the bleeding) and inflammation (the body's natural response to injury), focus on nutrients that support clotting and reduce inflammation. Vitamin K, found in leafy greens, is essential for clotting, while the antioxidants in berries help combat inflammation.
As your wound moves into the proliferation phase – the rebuilding stage – protein and Vitamin C become crucial. Protein, found in lean meats and fish, provides the building blocks for new tissue, while Vitamin C, abundant in citrus fruits, supports collagen production, the "scaffolding" for your new skin.
Creating the Optimal Healing Environment
Think of your wound as a delicate garden. You wouldn't leave it exposed to the elements, would you? Keeping the wound clean and properly dressed is paramount. Regular dressing changes, as advised by your healthcare provider, create a moist environment that promotes healing and protects against infection. How Home Wound Care Speeds Up Recovery offers further insights into this. This isn't about letting the wound "air out," but rather creating the optimal conditions for new tissue growth.
The Power of Rest and Stress Management
Sleep and stress management might seem unrelated to wound healing, but they play surprisingly important roles. Adequate sleep allows your body to focus its energy on repair. Imagine it like giving your construction crew the downtime they need to work efficiently. Chronic stress, on the other hand, can hinder your immune system and slow down healing. Techniques like deep breathing or meditation can help manage stress and support your recovery.
Movement and Circulation: Keeping the Supply Lines Open
Gentle movement and exercises, as recommended by your healthcare professional, are vital for good circulation. Good circulation ensures a steady supply of oxygen and nutrients reaches the wound site, like keeping the supply lines open to your body's construction crew. This is especially important for individuals with conditions like diabetes or peripheral artery disease, which can affect blood flow.
For comprehensive at-home wound care, consider Rapid Wound Care. They offer personalized treatments for various wound types, from chronic wounds to diabetic ulcers. Learn more at Rapid Wound Care.

