Understanding Why Patients Return to Your Hospital
Let's be honest—readmissions are more than just numbers on a quality report. They represent real patients who trusted you with their care and ended up back in your emergency department within weeks. To effectively reduce hospital readmission, we first need to dive deep into the "why." It's rarely a single, simple cause; instead, it's often a complex web of clinical, social, and logistical challenges that patients face after discharge.

Beyond the Diagnosis: The True Drivers of Readmission
While certain medical conditions are well-known for high readmission rates, focusing only on the diagnosis misses the bigger picture. Experienced nurses and case managers know that the reasons patients return are often hiding in plain sight, scattered across their medical charts, social histories, and even in brief bedside conversations. Think about the patient recovering from a complicated surgery. The procedure may have been a technical success, but what happens when they get home?
A successful recovery depends on a fragile ecosystem of support. A breakdown in any single part can send a patient spiraling back to the hospital. These breakdowns often fall into a few key categories:
- Clinical Setbacks: These are the medical issues we typically think of, like post-operative infections, unmanaged pain, or adverse reactions to new medications.
- Knowledge Gaps: The patient or their caregiver may not fully understand the discharge instructions, medication schedules, or critical warning signs that require a call to their doctor instead of a trip to the ER.
- Social and Economic Barriers: This is a huge, often overlooked category. Does the patient have reliable transportation for a follow-up appointment? Can they afford their new prescriptions? Is their home environment safe for someone with limited mobility?
Ignoring these social determinants of health is like trying to solve a puzzle with half the pieces missing.
Common Conditions and Their Hidden Risks
Certain patient populations are inherently at higher risk, and understanding their unique challenges is key to preventing their return. For example, heart failure (HF) is a leading cause of readmissions globally. A 2023 meta-analysis covering over 1.4 million HF hospitalizations found that the pooled 30-day readmission rate was a staggering 13.2%. Interestingly, the study noted that this high rate couldn't be explained by medical factors alone, pointing toward those very social and system-level issues we've been discussing. You can explore the full study about heart failure readmission variations on JACC.org.
To get a clearer picture of how these factors play out, let's compare the common reasons for readmission across different medical conditions. This table highlights not just the rates but the specific risk factors that care teams should focus on.
Readmission Rates by Medical Condition
Comparison of 30-day readmission rates across different medical conditions and specialties
| Medical Condition | 30-Day Readmission Rate | Primary Risk Factors | Prevention Focus |
|---|---|---|---|
| Heart Failure (HF) | 15-25% | Medication non-adherence, fluid/sodium mismanagement, lack of follow-up | Patient education on daily weights, diet, symptom recognition, and medication affordability programs. |
| Pneumonia | 15-20% | Lingering weakness, poor nutrition, co-existing conditions (like COPD), swallowing difficulties | Ensuring access to follow-up care, strength-building through physical therapy, and respiratory therapy education. |
| COPD | 20-25% | Environmental triggers (dust, smoke), incorrect inhaler technique, anxiety | Home environment assessment, proper inhaler training, and creating a clear action plan for exacerbations. |
As the table shows, while the medical conditions differ, the solutions often involve more than just medicine. They require education, support, and a practical approach to real-life barriers.
By shifting our perspective from just treating the disease to supporting the whole person, we begin to see readmissions not as unavoidable failures but as preventable events. Each return visit is an opportunity to learn what went wrong in that fragile post-discharge ecosystem and strengthen it for the next patient.
Spotting High-Risk Patients Before They Leave Your Unit
The best strategy for reducing hospital readmissions often starts long before a patient even thinks about their discharge papers. It’s a skill developed right at the bedside, not in a conference room. Identifying at-risk patients is about looking past the primary diagnosis to see the whole person—their home life, their support network, and how they’ll manage once they leave the controlled hospital environment. The aim isn't to be a fortune-teller; it's to catch the red flags that show a patient will need extra help and then stepping in to provide it.
Moving Beyond Clinical Scores
While formal risk assessment tools certainly have their place, many seasoned nurses and case managers know that real insight comes from keen observation. They've discovered that a patient's answers to a few straightforward, non-clinical questions can tell you more than a complicated algorithm ever could. For example, a patient with a new diagnosis might seem clinically stable, but if they live alone, don't have reliable transportation, or express worry about managing new prescriptions, their readmission risk just shot through the roof.
Integrating this kind of screening into your daily workflow is critical. It doesn't need to be another formal checklist. It can simply become part of the natural conversation during a medication round or a daily assessment. Some of the most valuable information comes from asking questions like:
- "Who's going to be at home to help you out for the first few days?"
- "Are you worried about getting or paying for your new medications?"
- "How are you planning to get to your follow-up appointment?"
These simple questions open a window into the social determinants of health that are powerful predictors of whether a patient can recover successfully at home.
High-Risk Conditions and Targeted Interventions
We know that certain diagnoses come with a higher chance of readmission, which means we need to be extra vigilant from day one. Recent data, for instance, shows that hospital stays for blood diseases have the highest readmission rates at 23.8 per 100 admissions, with cancers not far behind at 19.0 per 100 admissions. You can dig deeper into how clinical risk groups affect readmission rates on gkc.himss.org. These numbers tell us that patients with complex, systemic conditions often face a much more difficult recovery.
For these individuals, spotting risk early is everything. A patient getting chemotherapy might be clinically fine for discharge, but their compromised immune system makes them a prime target for infection at home. Likewise, a patient with a complex wound needs a clear, manageable care plan. If they don't have the physical ability or the support at home to perform dressing changes, readmission is almost guaranteed.
This is where specialized services can be a game-changer. By identifying this need before discharge, you can make a referral to ensure a professional continues their care at home, drastically cutting the risk of complications. Curious about how this works? You might be interested in learning about what mobile wound care is and why it's important for bridging this exact care gap.
Discharge Planning That Prepares Patients for Real Life
Let's move past the standard, one-size-fits-all discharge checklists. We need to talk about planning that actually holds up in the messy, complicated reality of a patient's life. The objective isn't just to check boxes for compliance; it's to build a realistic, actionable plan that helps reduce hospital readmission by setting patients up for success once they're back home. The best discharge planners understand that knowing a patient's real-world environment—where they live, who can help them, and what they can genuinely manage—is far more important than a perfectly reconciled medication list they can't afford.

From Hospital Chaos to Home Realities
Skilled healthcare teams know how to balance detailed planning with the immense time pressures of a busy hospital. They’ve learned that smooth transitions are no accident. They come from smart, targeted communication and a focus on what is truly important for the patient's recovery. This means we need to shift our focus from just giving information to making sure the patient understands it and feels capable of following through.
A primary cause of readmission is often simple confusion or feeling overwhelmed. Patients leave with stacks of papers detailing complex medication schedules, new dietary rules, and multiple follow-up appointments. Someone who just had major surgery is unlikely to remember half of what was said during a quick discharge conversation. This is where patient-centered techniques, like the "teach-back" method, become critical. Instead of asking, "Do you have any questions?" try this: "To make sure I did a good job explaining this, can you tell me in your own words how you'll take this new medicine?" This simple change can uncover understanding gaps that you can fix on the spot.
Creating a Realistic Post-Discharge Roadmap
A truly effective plan must account for life outside the hospital. It’s about building a solid bridge from the clinical setting to the patient’s home. This involves looking at a few key areas:
- Realistic Follow-Up: Is that follow-up appointment with a specialist across town, requiring two bus transfers for an elderly patient with mobility problems? If so, it’s not a realistic plan. Working with the patient’s existing primary care doctor or setting up in-home services can make a world of difference. For instance, ensuring continuity through effective post-discharge wound care at home can stop a minor issue from turning into a major reason for readmission.
- Practical Medication Management: The plan must address affordability and access. If a patient can't cover their copay, they won't fill the prescription. It's that simple. Connecting them with medication assistance programs or discussing lower-cost alternatives is a vital, proactive step.
- Emotional and Social Support: Recovery is hard work and can be emotionally draining. We need to acknowledge this and, with the patient's permission, involve family members or caregivers. They are a crucial support network that can help reinforce instructions and spot warning signs the patient might miss.
The Centers for Medicare & Medicaid Services (CMS) have put a major focus on this area. Their Hospital Readmissions Reduction Program (HRRP) highlights the importance of getting this right.

This screenshot shows the national priority placed on preventing readmissions, proving there are real financial and quality-of-care reasons for hospitals to improve their discharge planning. Ultimately, the key is to create discharge plans that patients want to and can follow, not just plans that tick boxes for documentation. This patient-first mindset is the foundation of any real strategy to reduce hospital readmissions.
Staying Connected Without Overwhelming Your Patients
The real work to reduce hospital readmission kicks in during those first vulnerable weeks after a patient goes home. This is when they're trying to recover while figuring out the often confusing world of home care. The most successful care teams have mastered the art of staying in touch during this critical time without making patients feel smothered or constantly monitored. It's a careful balance between being a resource and respecting their new-found independence.
The secret is purposeful follow-up. Not every call or message carries the same weight. Some interactions are incredibly effective at preventing readmissions, while others just make staff feel like they're "doing something." The most valuable follow-up is targeted, timely, and designed to uncover problems before they escalate.
Finding the Sweet Spot in Follow-Up Communication
Your goal is to build a safety net, not a surveillance system. Bombarding patients with calls can lead to "outreach fatigue," causing them to ignore important communications. A thoughtful approach always prioritizes quality over quantity. For example, a single, well-timed call from a nurse who can answer specific questions about medication is far more helpful than three automated check-in texts.
Research consistently shows that patients who receive post-discharge follow-up have much better outcomes. One study of a community hospital's outreach program found that patients who reported feeling worse after discharge had a 17.2% readmission rate, and those who couldn't get a ride to follow-up appointments had a 29.1% readmission rate. Catching these specific issues with a simple phone call can change everything.
This infographic shows just how much effective follow-up can move the needle on readmissions while keeping patients engaged.
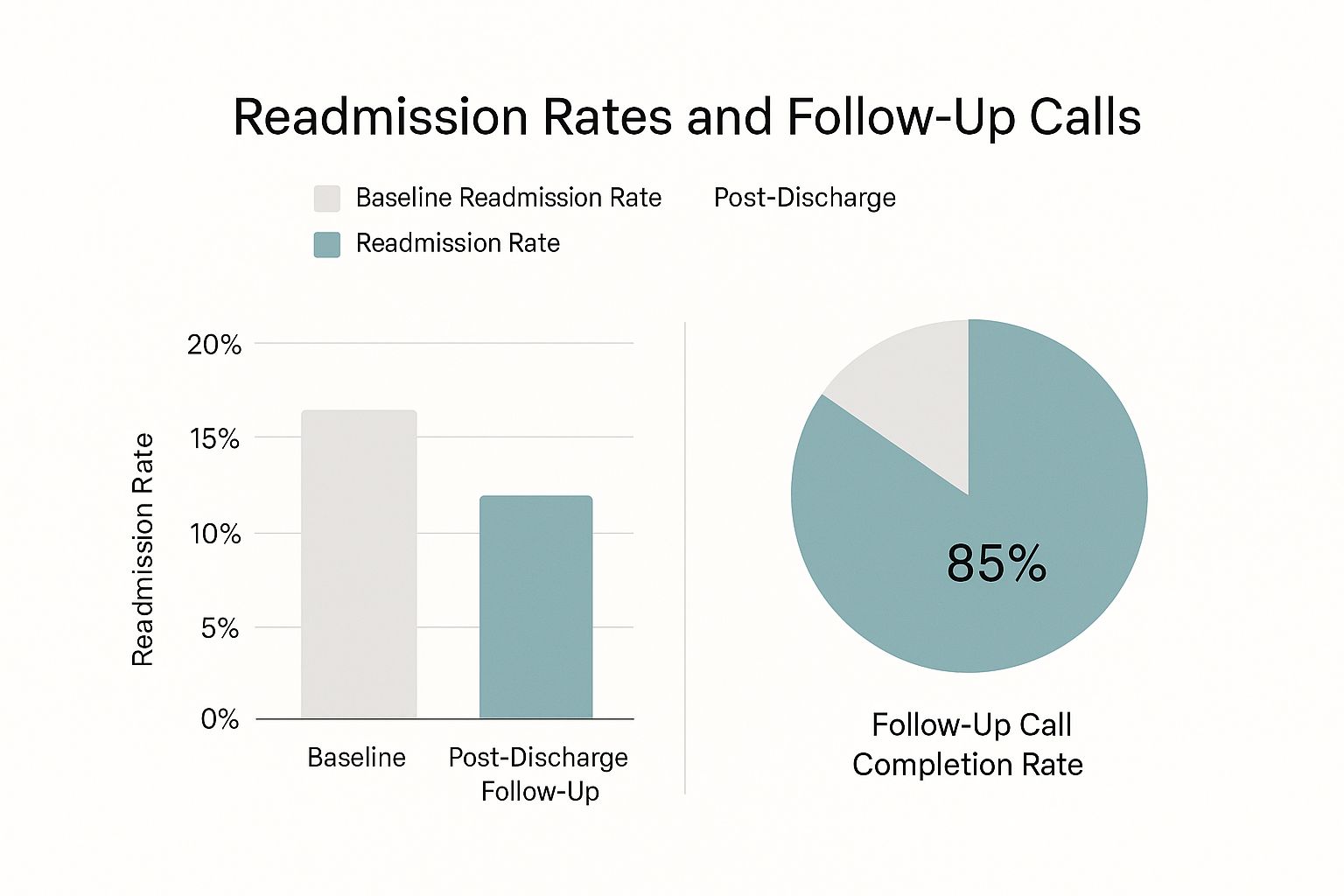
The data is clear: a one-third drop in readmissions for patients who get follow-up contact. This demonstrates the direct impact of staying connected.
To help structure this process, we've outlined a timeline for post-discharge contacts. This table details when to reach out, what method to use, and what to focus on during each interaction.
| Contact Type | Timing After Discharge | Method | Key Focus Areas | Success Metrics |
|---|---|---|---|---|
| Initial Check-in | 24-72 hours | Phone Call | Medication reconciliation, confirming appointments, asking about any immediate warning signs or symptoms. | Patient confirms understanding of care plan; no urgent issues identified. |
| PCP Communication | Within 48 hours | Secure Email/EHR Message | Sending a concise discharge summary, highlighting key care plan elements and follow-up needs. | PCP acknowledges receipt and confirms patient's scheduled follow-up visit. |
| Mid-Week Check-in | Days 5-7 | Phone Call or Secure Text | Probing for new issues (pain, confusion), checking on transportation for follow-up, reinforcing education. | Patient reports stable condition; transportation for appointments confirmed. |
| Home Health Coordination | Before first visit | Phone Call/Secure Message | Confirming start date, sharing specific wound care orders or patient needs, establishing a point of contact. | Home health agency confirms services are scheduled and initiated on time. |
| Pre-PCP Visit Reminder | 24 hours before 1st PCP appt. | Automated Text/Call | Reminding patient of appointment time/location, asking them to bring their medication list and questions. | Reduced "no-show" rate for first post-discharge PCP appointment. |
This structured approach ensures that communication is not only timely but also highly relevant to the patient's recovery stage. By tailoring the method and focus, you create a more effective and less intrusive support system.
Building a Coordinated Communication Web
True success in follow-up isn't just about contacting the patient. It's about creating a communication web that includes primary care providers (PCPs), specialists, and trusted community partners. One of the biggest failures in care transition is when a patient's PCP has no idea they were even in the hospital. A direct, simple communication from your team to the PCP, summarizing the hospital stay and care plan, is a powerful and often overlooked tool.
Here's a practical way to think about who to contact and why:
- The Patient/Caregiver (24-72 hours post-discharge): This is your most important check-in. The conversation should center on medications, upcoming appointments, and any immediate red flags. Ask open-ended questions like, "How are you feeling compared to when you left the hospital?" instead of a simple "Are you feeling okay?"
- The Primary Care Provider (within 48 hours): Send a clear, concise discharge summary. This ensures the PCP is in the loop and can reinforce the hospital's care plan during the patient’s first visit.
- Home Health Services (if applicable): Coordination here is absolutely vital. You need to confirm that skilled nursing or therapy services are scheduled to start on time to prevent any gaps in care. If you want to dive deeper into this area, you can explore the reasons home health care is essential for a patient's recovery.
By thoughtfully organizing these touchpoints, you build a strong support system that catches problems early. This proactive, team-based approach is the foundation of a lasting strategy that not only lowers readmission numbers but truly improves patient safety and well-being after they leave your facility.
Teaching Patients What They Actually Need to Know
Patient education is often where great intentions collide with disappointing results. We’ve all seen it: handing someone a thick folder of pamphlets written at a college reading level just moments before they leave the hospital. That isn’t a strategy—it’s a formality. To genuinely reduce hospital readmission, we have to shift from information-dumping to meaningful teaching that actually sticks.
The most effective educators understand that a patient's ability to learn is heavily influenced by stress, health literacy, and their cultural background. The secret isn’t to teach them everything; it's to teach them the critical few things they absolutely must know to stay safe at home. Our goal is to distill complex medical information into simple, actionable steps that someone who is tired, sore, and overwhelmed can remember and follow.
The "Teach-Back" Method: Confirming Understanding, Not Testing Knowledge
One of the most powerful tools in a clinician's toolkit is the teach-back method. It fundamentally changes the dynamic from a one-way lecture to a two-way conversation. More importantly, it places the burden of clear communication on the provider, not the patient.
Instead of asking a closed-ended question like, "Do you understand your new medication schedule?" which almost always gets a simple "yes," you reframe it. A nurse could say:
- "We went over a lot of information about your new heart medication. To make sure I did a good job explaining it, can you tell me in your own words when you're supposed to take it and what you should watch out for?"
This simple change is profound. It’s not a test of the patient’s memory; it’s a check on your teaching effectiveness. If they can't explain it back, you know you need to try again with a different approach. Research has shown that when patients don't understand their discharge instructions, the consequences are severe. One study found that for heart failure patients, having unclear instructions was associated with a 28.3% readmission rate. This shows just how urgent it is to confirm comprehension before they walk out the door.
Focusing on the "Need-to-Know" vs. "Nice-to-Know"
A patient recovering from pneumonia doesn't need a biology lesson on how bacteria invade the lungs. What they do need to know is much more practical and immediate. The key is to prioritize information based on what poses the biggest risk for readmission.
Let's break down what this looks like for a common diagnosis, like post-surgery wound care:
| Priority Level | What to Teach (Example: Post-Surgery Wound Care) |
|---|---|
| Must-Know (Top Priority) | How to spot signs of infection (like redness, pus, or a fever) and who to call immediately. How to properly change the dressing. |
| Should-Know (Important) | What activities to avoid (heavy lifting, soaking in a tub). How to manage pain with prescribed medication. |
| Nice-to-Know (Can Wait) | The cellular process of tissue granulation. The full list of every possible, but rare, complication. |
By zeroing in on the "Must-Know" items, you give patients the critical knowledge they need to manage their immediate safety. Involving family members or a designated caregiver in these conversations is also crucial, as they can act as a second set of ears and a support system at home. Always ask the patient for permission first, but framing it as building their "care team" often helps.
This focused, collaborative approach to education doesn't just lower the risk of readmission—it empowers patients to become active partners in their own recovery.
Learning From Hospitals That Get It Right
Some hospitals consistently keep their readmission rates low, while others seem to be in a constant battle, even when they have similar patient groups and resources. So, what sets the successful ones apart? It's almost never a single "aha!" moment but a deliberate, systematic approach to care that they refine over time. By examining these high-performing organizations, we can uncover practical strategies to reduce hospital readmission that are much more effective than just ticking boxes on a discharge checklist.

From Policy Pressure to Practical Change
Let's be honest, external pressure, especially from government initiatives, has played a big role. The Hospital Readmissions Reduction Program (HRRP) from the Centers for Medicare & Medicaid Services (CMS) definitely got hospitals to pay attention. The results are showing: for the 2025 fiscal year, only 7% of hospitals face Medicare payment cuts of 1% or more because of readmissions. That's an improvement from 7.5% the previous year and a five-year low, which proves focused efforts work. You can get more details on these recent readmission penalty trends on Advisory.com.
But here’s the key difference: the best hospitals don't just react to policy changes. They use them as a springboard for real, meaningful improvements. They stop "teaching to the test" and start embedding prevention into their everyday culture. They figured out that lasting success comes from empowering their staff, not just piling on more protocols and causing burnout.
Common Threads of Successful Programs
Whether it's a huge academic medical center or a small rural hospital, the successful programs share some common DNA. They tend to focus on a few key areas that give them the biggest bang for their buck.
- Data-Driven Decision Making: Top performers are obsessed with their data. They don't just glance at the overall readmission rate. They dig deeper to find out which units, which diagnoses, and sometimes even which physicians are linked to higher rates. This helps them direct their efforts exactly where they are needed most.
- Empowered Frontline Staff: These hospitals trust the people on the ground—their nurses, therapists, and case managers. They give them the freedom to make quick decisions, like arranging for an in-home care visit or getting a social worker involved to solve a patient's transportation problem before it becomes a crisis.
- Strong Community Partnerships: No hospital is an island. The most effective programs create solid relationships with primary care doctors, skilled nursing facilities, and home health agencies. This creates a smooth transition for patients, making sure no one falls through the cracks. For instance, a solid partnership with a mobile wound care service can be a game-changer for a patient with a complex surgical wound, directly affecting their recovery and keeping them safely at home. You might find our guide on how home health wound care improves patient outcomes helpful.
The most valuable lessons come from seeing the real-world challenges these hospitals ran into and how they solved them. They learned which strategies created lasting change and which ones were just a temporary fix. Their journeys show that lowering readmissions is a marathon, not a sprint. It’s built on constant improvement and a genuine commitment to a patient’s well-being long after they've left the hospital.
Building Your Readmission Prevention Program
Now, let's turn all this theory into a practical game plan you can start using right away. Whether you're building a program from scratch or tweaking an existing one, the goal isn't overnight perfection. It's about making real, steady progress that helps patients and works with the resources you already have. The trick is to build momentum with small victories as you work toward bigger, system-wide improvements.
Kicking Off Your Program: First Steps and Early Wins
Getting started can feel like a huge task, but you don’t need a massive budget or a whole new department. The best approach is to start small and identify your biggest opportunities for impact. Dive into your hospital’s data: which patient groups or units have the highest 30-day readmission rates? Often, patients with heart failure, COPD, or those recovering from surgery are good places to start.
Once you’ve zeroed in on a target group, pull together a small, multidisciplinary "sprint team." This team shouldn't just be managers; it needs champions from the front lines who live the day-to-day realities of patient care.
- Your Sprint Team Roster:
- A motivated floor nurse who has the respect of their peers.
- A dedicated case manager or social worker who truly understands the barriers patients face at discharge.
- An engaged pharmacist to help sort out medication issues, from reconciliation to cost concerns.
- A physician or specialist champion who can be a strong voice for the program.
Your first goal is to implement one or two changes that are high-impact but low-effort. For example, you could pilot the teach-back method on a single unit for every patient discharged with heart failure. Or, you could standardize a post-discharge follow-up call script and have a case manager call just five high-risk patients a week. These early successes create the proof of concept you need to get broader support and more resources down the line.
Engaging Stakeholders and Securing Buy-In
To grow your pilot into a hospital-wide initiative, you need support from leadership and other departments. Don't just show up with problems; present them with solutions backed by your pilot data. Frame your proposal around the benefits that resonate with them: better quality metrics, lower financial penalties from programs like the HRRP, and higher patient satisfaction scores.
When you talk to department heads, try to anticipate their concerns. A common worry is that new protocols will just add to their staff's already heavy workload. Address this by showing how your program can fit into existing workflows instead of adding clunky new steps. A standardized post-discharge call isn't an "extra" task; it’s a more structured and effective way of doing what great case managers already try to do.
Training is also key. Instead of one long, overwhelming training session, introduce new practices in smaller doses. Use short huddles on the unit and encourage peer-to-peer coaching. A nurse champion showing a colleague how to use the teach-back method is much more powerful than a formal lecture.
Measuring What Matters and Adapting Your Approach
Think of your program as a living thing that needs to adapt based on what the data is telling you. You'll want to track both process measures (are we doing the things we said we would?) and outcome measures (are those things actually working?).
| Metric Type | Example Metric | Why It Matters |
|---|---|---|
| Process Measure | % of high-risk patients getting a follow-up call within 72 hours. | Shows if your team is successfully putting the new process into action. |
| Outcome Measure | 30-day readmission rate for your target patient group. | Shows if your efforts are actually working to reduce hospital readmission. |
| Balancing Measure | Staff satisfaction scores on the pilot unit. | Makes sure you're not lowering readmissions by burning out your team. |
By keeping an eye on these metrics, you can celebrate wins, figure out what isn't working, and make smart adjustments. Maybe you find your follow-up calls aren't catching key problems. That insight might lead you to tweak your script or change when you make the calls. For certain patients, especially those with complex wounds, a phone call might not be enough. This is where proactive coordination for specialized services becomes crucial. As detailed in our guide on how wound care in Chicago is delivered, bringing care directly to a patient's home can be a game-changer.
If your facility is struggling with complex wounds after discharge, don't let those patients get lost in the system. The team at Rapid Wound Care can offer the specialized, in-home support needed to promote proper healing and stop a preventable readmission before it happens.

