Understanding The Real Impact of Pressure Injuries
Pressure injuries, also known as pressure ulcers or bedsores, present a significant challenge in healthcare. These injuries occur when constant pressure on the skin restricts blood flow, damaging the underlying tissue. Anyone can develop a pressure injury, but individuals with limited mobility, like those in hospitals or long-term care facilities, are particularly vulnerable. In fact, hospital-acquired pressure injuries (HAPIs) affect more than one in ten hospitalized adults. The persistence of this issue, despite advancements in healthcare, highlights the urgent need for effective preventative measures. Learn more about pressure injury statistics here.
The Human Cost of Pressure Injuries
Beyond the numbers, it's crucial to understand the significant impact these injuries have on individual lives. Pressure injuries can cause considerable pain and discomfort, restricting movement and limiting participation in everyday activities. This can lead to a diminished quality of life, even contributing to feelings of isolation and depression. Furthermore, infections can develop in these wounds, increasing the risk of serious complications and extending recovery times. A seemingly minor pressure injury can quickly escalate into a serious health concern requiring extensive medical intervention.
The Burden on Healthcare Systems
Pressure injuries place a substantial strain on healthcare systems globally. The costs associated with treating these wounds, including specialized dressings, medications, and sometimes surgery, are substantial. Extended hospital stays, often a consequence of pressure injuries, further increase the financial burden on both the healthcare system and the patient. Therefore, effective pressure injury prevention is not just about patient well-being; it's a critical aspect of managing healthcare costs. Learn more about pressure injury prevention here.
Vulnerable Populations
Certain groups face a higher risk of developing pressure injuries. Older adults, individuals with chronic conditions such as diabetes or spinal cord injuries, and those with limited mobility are particularly susceptible. This elevated risk underscores the importance of targeted prevention strategies for these populations. Malnutrition and weakened immune systems can also increase a person's vulnerability. However, with proper care and proactive measures, many pressure injuries are preventable.
The Financial Reality Behind Prevention Programs

The financial strain of pressure injuries on healthcare systems is immense, frequently surpassing dedicated wound care budgets. This makes pressure injury prevention not only a medical necessity but a financial one. Astute healthcare leaders understand that prioritizing prevention safeguards their financial resources.
The High Cost of Treatment
Treating pressure injuries incurs substantial costs, including specialized dressings, medications, and potential surgeries. These direct costs are just the beginning. Extended hospital stays, increased nursing hours, and the need for specialized equipment and therapies add to the financial burden. These hidden costs accumulate rapidly, significantly impacting a facility's resource allocation. For helpful insights, check out How to master home health wound care.
Prevention as a Financial Strategy
Progressive administrators recognize that preventing pressure injuries is far more economical than treating them. The estimated national cost for treating Hospital-Acquired Pressure Injuries (HAPIs) in the U.S. ranges from $3.3 billion to $11 billion each year.
The global pressure ulcer prevention market, valued at approximately $1.12 billion in 2024, is projected to expand due to increased awareness and the demand for cost-effective solutions. Learn more about this market growth here. Investing in pressure injury prevention programs can significantly reduce these considerable financial strains.
Building a Business Case for Prevention
Creating a compelling business case for pressure injury prevention involves showcasing a clear return on investment (ROI). This entails calculating current treatment costs and comparing them to the projected costs of preventative measures. By highlighting how prevention can shorten hospital stays, reduce nursing time, and minimize the need for expensive interventions, administrators can effectively advocate for resources. This positions pressure injury prevention not as an additional expense, but as a strategic investment in financial stability and improved patient outcomes.
Mastering Risk Assessment and Early Detection
Effective pressure injury prevention starts with identifying at-risk individuals before injuries appear. This means understanding traditional risk factors and new indicators revealed by recent research. Putting consistent and accurate risk assessment procedures in place is key for turning risk identification into effective prevention.
Essential Risk Assessment Tools
Several tools help healthcare professionals evaluate pressure injury risk. The Braden Scale, for instance, is widely used and considers factors like sensory perception, moisture, activity, mobility, nutrition, and friction/shear. Other assessments, such as the Norton Scale and the Waterlow Scale, also offer valuable insights into individual patient risk.
- Braden Scale: Assesses sensory perception, moisture, activity, mobility, nutrition, and friction/shear.
- Norton Scale: Evaluates physical condition, mental state, activity, mobility, and incontinence.
- Waterlow Scale: Considers build/weight for height, skin type, sex, age, continence, mobility, and appetite.
Selecting the appropriate assessment tool depends on the specific patient group and the healthcare setting. For further reading, check out the official resources for the Braden Scale, the Norton Scale, and the Waterlow Scale.
To help visualize the differences between these tools, the following table provides a quick comparison.
Pressure Injury Risk Assessment Comparison: This table compares commonly used pressure injury risk assessment tools, their effectiveness, and ideal patient populations.
| Assessment Tool | Sensitivity Rate | Best Used For | Implementation Time |
|---|---|---|---|
| Braden Scale | Varies widely (60-90%) | All patient populations | ~5-10 minutes |
| Norton Scale | Lower than Braden Scale | Elderly patients, critical care | ~2-5 minutes |
| Waterlow Scale | Comparable to Braden Scale | Patients with acute or chronic illnesses | ~5-10 minutes |
Key differences emerge when considering the sensitivity and implementation time. While the Braden and Waterlow scales offer higher sensitivity, they take a bit longer to administer. The Norton Scale, while quicker, may not be as sensitive in identifying all at-risk individuals.
Implementing Effective Screening Processes
Comprehensive screening processes should fit smoothly into existing workflows without overwhelming staff. Regular skin assessments, done on admission and at least daily afterward, are essential. These assessments should note skin condition, focusing particularly on bony prominences.
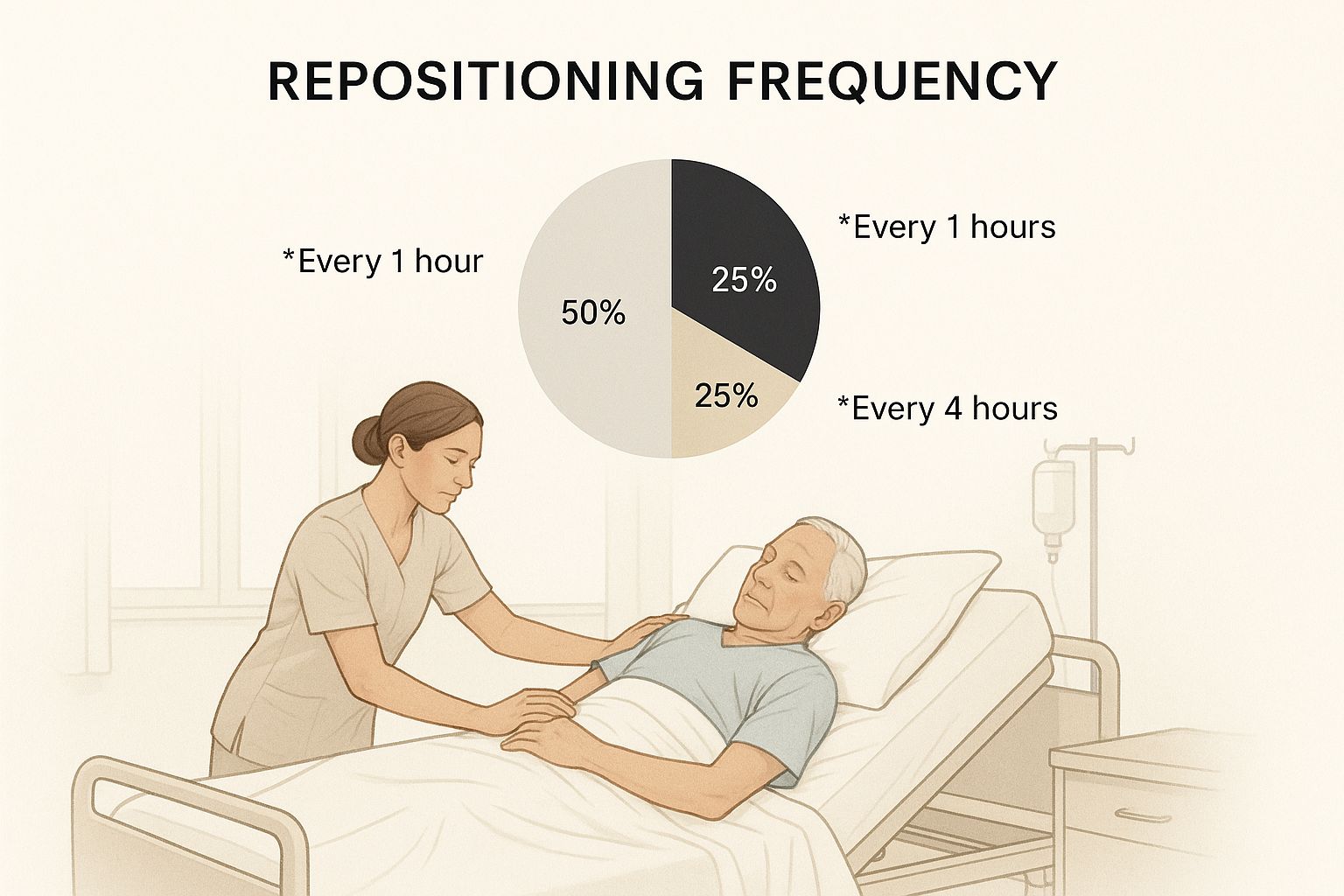
This image shows the 30-degree lateral tilt repositioning technique, a critical part of pressure injury prevention. Regular repositioning, as seen here, helps distribute pressure and lower the risk of skin breakdown. This is especially important for patients with limited mobility. For more information on home care for pressure ulcers, check out this article: How to master pressure ulcer treatment in home care.
Utilizing Digital Tools and Technologies
Technology is changing early detection and monitoring. Digital tools can automate risk assessments, follow skin changes over time, and send real-time alerts to healthcare providers. These improvements increase accuracy, consistency, and communication across different shifts and departments.
Addressing Common Assessment Pitfalls
Several things can affect the accuracy of risk assessments. Incomplete documentation, inconsistent use of assessment tools, and insufficient staff training can lead to missed prevention opportunities. Regularly reviewing assessment practices and offering continuous education for healthcare professionals are essential for maintaining accuracy and effectiveness in pressure injury prevention. Tackling these challenges directly ensures that risk assessments result in effective prevention strategies. For example, studies show that evidence-based nursing interventions, including regular turning and using pressure-redistributing support surfaces, significantly reduce the occurrence of pressure injuries in intensive care unit patients compared to standard nursing interventions.
Choosing Prevention Technologies That Actually Work
The sheer number of pressure injury prevention technologies can be overwhelming. Many products promise amazing results, making it tricky to separate truly effective solutions from clever marketing. This section helps clarify things, focusing on technologies with proven success in real-world healthcare settings.
From Smart Mattresses to Advanced Dressings
Innovative prevention tools range from smart mattresses with pressure mapping to advanced wound dressings. Pressure mapping creates a visual representation of pressure distribution, allowing caregivers to pinpoint high-pressure areas and adjust patient positioning. Some smart mattresses even automatically adjust internal air pressure to redistribute pressure and minimize risk.
Specialized dressings also play a vital role. These dressings do more than just cover the wound; they actively create an environment that promotes healing. Some include antimicrobial agents to prevent infection, while others use materials that encourage tissue regeneration.
A community hospital study revealed significant differences in average annual Hospital-Acquired Pressure Injury (HAPI) incidence based on the type of silicone foam dressing used. One dressing resulted in 10.40 HAPIs per year, another in 5.56, and a third in 26.29. This highlights how dressing selection significantly impacts patient outcomes. One dressing even saved an estimated $451,229.91 compared to another. More detailed statistics can be found here.
Evaluating Effectiveness: Beyond the Sales Pitch
Choosing the right technology requires a critical eye, prioritizing real-world evidence over marketing claims. Speaking with healthcare professionals who have direct experience using these technologies offers invaluable insights. Consider factors like patient comfort, ease of use for staff, and how well the technology integrates with existing equipment and workflows. This practical approach helps determine a technology's true value.
Essential Criteria for Product Selection
Cost-effectiveness is essential when evaluating prevention technologies. While some may have a higher upfront cost, their ability to prevent expensive pressure injuries can lead to long-term savings. Look beyond the product price and consider the total impact on resource use, including nursing time, dressing changes, and treating complications. This gives a complete view of the true cost of care.
Emerging Technologies and Future Trends
Beyond established technologies, new innovations hold great promise. Artificial intelligence (AI) is being used to predict high-risk patients, enabling targeted interventions. Wearable sensors can continuously monitor pressure points, alerting caregivers to potential issues before they become visible. These advancements offer exciting opportunities to further reduce pressure injury rates. The practical implementation and long-term effectiveness of these innovations are still being assessed.
Avoiding Common Technology Adoption Mistakes
Implementing new technologies requires careful planning and execution. Just buying a new mattress or dressing isn’t enough. Success depends on integrating the technology into current workflows and properly training staff on its effective use. Consistent monitoring and evaluation are crucial to track the impact and find areas for improvement. A well-planned approach maximizes the benefits of the technology and ensures a positive return on investment. This ensures that your investment leads to noticeable improvements in patient care.
Building Prevention Protocols That Stick
Creating effective pressure injury prevention protocols is crucial, but ensuring their consistent use in a busy healthcare environment can be tough. This means balancing staff limitations and other important tasks to create practical, sustainable solutions. Let's explore how to build pressure injury prevention programs that truly make a difference, using real-world examples and proven methods.
Practical Protocol Development
Effective protocols address key areas like repositioning schedules, nutrition management, skin care routines, and proper equipment use.
- Repositioning: Create clear guidelines for how often patients should be repositioned, including specific techniques like the 30-degree lateral tilt, to relieve pressure on bony areas.
- Nutrition: Encourage enough protein and fluids to support healthy skin and wound healing.
- Skin Care: Implement regular skin assessments and cleansing routines, using moisture barriers to protect vulnerable spots.
- Equipment: Ensure proper use of support surfaces like special mattresses and cushions to distribute pressure evenly.
Keep staff capabilities and patient comfort in mind when designing these protocols. Involving nurses and other healthcare professionals in the creation process builds support and improves adherence.

Overcoming Implementation Barriers
Staff shortages and workflow interruptions are common obstacles in implementing pressure injury prevention programs. Overcoming these challenges requires resourceful solutions and solid support from leadership.
- Staffing: Cross-train staff to ensure sufficient coverage for repositioning and skin care. Think about assigning specific tasks to trained aides or assistants.
- Workflow: Incorporate prevention measures into current workflows to minimize disruptions and increase efficiency. Use checklists and reminders to encourage adherence to the protocols.
- Leadership Support: Secure support from leadership to provide the necessary resources and make pressure injury prevention a priority within the organization.
Maintaining Program Effectiveness Over Time
Sustaining a successful pressure injury prevention program requires continuous monitoring and adjustments. Regularly review program data, including pressure injury rates and how well staff follow protocols, to pinpoint areas for improvement. Ongoing staff training and education reinforce best practices and make sure everyone stays informed about the latest evidence-based methods. You may find this helpful: What is Mobile Wound Care and Why is it Important?
Adapting to Specific Needs
Each healthcare facility faces its own set of challenges. Tailoring your approach based on these specific factors ensures program success. For instance, a long-term care facility may focus on nutrition and skin care because of more immobility and chronic conditions, while an acute care hospital might emphasize early risk assessment and frequent repositioning for patients having surgery or in intensive care. Regularly assess program effectiveness and adjust as needed, based on patient requirements and resources. Open communication among staff, combined with a focus on continuous improvement, ensures your pressure injury prevention program stays a dynamic and effective tool for better patient care. This flexible approach leads to a truly impactful and lasting program.
What's Coming Next In Prevention Innovation
The field of pressure injury prevention is constantly advancing, driven by new technologies and the evolving needs of patients. Rather than chasing short-lived fads, let's examine the truly significant shifts in prevention strategies. We'll explore how artificial intelligence (AI), wearable sensors, and predictive analytics are already making a difference, using real-world cases. Understanding these developments helps us prepare for the future of pressure injury prevention.
The Rise of AI and Predictive Analytics
AI is set to reshape how we identify and manage pressure injury risk. Algorithms can analyze patient information, including medical history, vital signs, and even skin images, to pinpoint individuals most at risk. This early identification enables prompt interventions, potentially preventing injuries before they occur. This targeted approach allows resources to be directed towards those who need them most, improving both patient care and resource management. Predictive analytics empowers healthcare professionals to make data-driven decisions about prevention strategies, personalizing care for individual patients.
Wearable Sensor Technology: Continuous Monitoring
Wearable sensors present another promising avenue for pressure injury prevention. These small, discreet devices continuously track pressure on vulnerable areas, sending real-time alerts to caregivers if pressure reaches dangerous levels. This allows for quick adjustments to patient positioning or support surfaces, preventing prolonged pressure that can lead to skin breakdown. Continuous monitoring is particularly beneficial for patients unable to express discomfort or those at high risk due to limited mobility.
Market Forces Driving Innovation
Several factors are accelerating the development and adoption of new prevention technologies. The aging population, with its increased vulnerability to pressure injuries, is a significant driver. The pressure ulcer device market is expected to expand at a 5.6% compound annual growth rate through 2034, reaching $9.38 billion by 2034 from $5.46 billion in 2024. This growth reflects the rising demand for effective prevention devices and methods. Learn more about the growing pressure ulcer device market here. Policy changes and reimbursement models that incentivize prevention also play a crucial role.
Preparing for the Future of Prevention
Healthcare organizations can take proactive steps to integrate these emerging technologies. Investing in staff training on new technologies and incorporating them into current workflows is crucial for maximizing their effect. Collaboration across different healthcare disciplines, such as nurses, physicians, and wound care specialists, will become increasingly vital for creating comprehensive prevention strategies. By embracing these advancements and adapting to the changing healthcare environment, organizations can strengthen their pressure injury prevention programs and enhance patient outcomes.
Your Action Plan For Prevention Success
Ready to improve your pressure injury prevention strategy? This section provides a practical roadmap to develop and implement a successful program. We'll break down the essential components into actionable steps you can begin immediately. From securing initial support to measuring success, we'll equip you with the tools healthcare professionals use to make a real difference.
Building Your Prevention Program: A Step-by-Step Guide
Creating a successful pressure injury prevention program requires a structured approach. Here’s a practical framework to guide you:
-
Secure Organizational Support: Begin by presenting a compelling case highlighting the financial and patient care benefits of prevention. This is essential for gaining leadership buy-in and securing necessary resources.
-
Conduct a Needs Assessment: Evaluate your facility's current pressure injury rates, patient demographics, and existing resources. This assessment helps tailor your program to your facility’s specific needs.
-
Develop Clear Protocols: Establish clear guidelines for risk assessment, skin care, repositioning, nutrition, and support surface use. Ensure these protocols are practical for your team to implement consistently.
-
Provide Comprehensive Training: Equip your staff with the knowledge and skills to effectively implement the prevention program. Ongoing training reinforces best practices and ensures everyone stays up-to-date.
-
Implement and Monitor: Roll out your program gradually, closely monitoring its progress. Make necessary adjustments based on feedback and collected data.
To illustrate a practical implementation plan, let's review a sample timeline. The following table outlines key activities, success metrics, and resources required for each phase of implementation.
Prevention Program Implementation Timeline
Month-by-month action plan for implementing a comprehensive pressure injury prevention program in healthcare facilities
| Timeline | Key Activities | Success Metrics | Resources Needed |
|---|---|---|---|
| Month 1 | Secure leadership buy-in, conduct needs assessment | Budget approval, completion of needs assessment report | Administrative support, data analysis tools |
| Month 2 | Develop protocols, select prevention technologies | Finalized protocols, purchase orders for equipment | Clinical expertise, vendor collaboration |
| Month 3 | Staff training, pilot program launch | Staff competency scores, initial program data | Training materials, dedicated staff time |
| Months 4-6 | Ongoing monitoring, data analysis, program adjustments | Reduction in pressure injury rates, improved adherence to protocols | Data tracking tools, regular team meetings |
This timeline provides a basic framework. Remember to adjust it based on your facility’s specific circumstances and available resources. Regularly reviewing and updating your plan will be key to long-term success.
Measuring Success and Demonstrating Value
Tracking key metrics demonstrates your program’s effectiveness and justifies continued investment. Focus on these essential indicators:
-
Pressure Injury Incidence Rates: Track changes in the number of new pressure injuries. This directly demonstrates the impact of your prevention efforts.
-
Adherence to Protocols: Monitor how well staff follow established guidelines. This reveals how effectively the program integrates into daily practice.
-
Cost Savings: Analyze reductions in treatment costs and hospital stays. This data highlights the financial benefits of prevention to administrators.
-
Patient Satisfaction: Gather patient feedback regarding their comfort and overall experience. This humanizes the program’s impact and underscores its value.
Avoiding Common Pitfalls
Be aware of common challenges to ensure your program’s lasting success. Proactive planning can help you navigate these potential obstacles.
-
Lack of Staff Buy-In: Address staff concerns, provide adequate training, and showcase early successes to encourage engagement and participation.
-
Inconsistent Implementation: Establish clear protocols, use checklists and reminders, and provide regular feedback to ensure consistency.
-
Inadequate Monitoring: Consistently track key metrics. Regularly analyze the data, adapting the program as needed to achieve desired outcomes.
Check out our guide on How to master home wound care to speed up recovery for more information on accelerating healing and improving patient outcomes.
Ready to take your pressure injury prevention to the next level? Rapid Wound Care provides expert, at-home wound care services, including specialized treatment for pressure injuries. Learn more about how we can partner with you to achieve exceptional patient outcomes at Rapid Wound Care.

