Understanding Medicare Home Health: Your Care Safety Net
Imagine having a dedicated medical team that comes directly to your living room, turning it into a space of healing and recovery. This isn't a futuristic concept; it's the core promise of Medicare home health benefits. This program acts as a vital safety net, delivering skilled medical care in the one place most people feel safest and most comfortable: their own home. It represents a move away from relying only on sterile, institutional settings and toward a more personal, dignified approach to healthcare.
This preference for at-home care isn't just a feeling. The data reveals a powerful trend toward aging in place, supported by Medicare. Each year, around 12 million Americans receive home health care, and Medicare covers the cost for approximately 42% of these visits. With about 86% of home health patients being 65 or older, it's clear this benefit is a cornerstone of senior healthcare. In fact, when given the choice, nearly 90% of patients choose to receive care at home rather than in a facility—a strong indicator of the desire for independence. You can find more details in these home health statistics that highlight its impact on patient care.
Home Health vs. Traditional Settings
So, what makes home health care such a popular choice? The difference is about more than just convenience. While hospitals and clinics are critical for acute health crises, home health focuses on continuing that high level of care during recovery and for managing long-term conditions. Professionals can deliver everything from complex wound care to physical therapy using your own environment—like your kitchen table—as their workspace. This integration into daily life is a key advantage. You can learn more about the fundamental reasons home health care is essential for modern patient recovery.
To better understand the differences, the table below contrasts the patient experience and outcomes between home health and more traditional healthcare environments.
Medicare Home Health vs. Traditional Healthcare Settings
Comparison of care delivery, patient satisfaction, and outcomes between home health and institutional care
| Care Setting | Patient Satisfaction Rate | Average Cost | Recovery Time | Readmission Rate |
|---|---|---|---|---|
| Medicare Home Health | Generally Higher | Lower than Hospital Stays | Often Faster | Typically Lower |
| Hospital/Inpatient | Varies | Higher | Dependent on Condition | Higher for some conditions |
| Skilled Nursing Facility | Variable | Moderate to High | Varies by patient | Can be higher than home |
As the table shows, home health often leads to better patient satisfaction and lower readmission rates, all while being more cost-effective than a hospital stay. This approach allows for a recovery that is both efficient and centered on the patient's well-being.
The Human Element of Home Care
Beyond the statistics and comparisons, the real power of Medicare home health benefits is in the human connection. It's about maintaining family ties, preserving a sense of normalcy, and giving patients the ability to be active participants in their own recovery. When a nurse helps manage medications in a familiar setting or a therapist adapts exercises to a patient's own living space, the care becomes more effective and less disruptive. This approach has been shown to reduce hospital readmissions and improve overall quality of life, allowing patients to heal where they feel they truly belong.
Qualifying For Medicare Home Health: The Four Gates
Think of qualifying for Medicare home health benefits as needing to unlock four different gates. You need the right key for each one, and only with all four can you access the full range of services. Many people get discouraged because they misunderstand these rules, but the requirements are often more flexible than they appear. Let's walk through them one by one.
Gate 1: Doctor's Certification and Plan of Care
The foundation of your eligibility is your doctor's official certification. A physician, nurse practitioner, or physician assistant must formally state that you require skilled medical care at home. This isn't just a simple note; it's a detailed plan of care.
Imagine this plan as a roadmap for your recovery. It outlines the specific services you need, how often you'll receive them, and the health goals everyone is working toward. This crucial document must be reviewed and re-certified by your doctor at least every 60 days. Your doctor's active involvement is a must-have, as it proves the medical necessity of your care.
Gate 2: The Need for Skilled Services
The second gate requires you to need intermittent skilled nursing care or therapy services. "Intermittent" means part-time or periodically, not around-the-clock care. The key word here is "skilled," which refers to care that can only be performed safely and correctly by a licensed professional.
Examples of skilled services include:
- Administering intravenous (IV) drugs
- Complex wound care for pressure ulcers or surgical wounds
- Giving injections
- Physical, occupational, or speech therapy
It's a common myth that you're disqualified if you have a family member willing to help. A loved one, no matter how dedicated, is not a substitute for a licensed professional. Needing a skilled service, even just a few times a week, is enough to open this gate to Medicare home health benefits.
This infographic illustrates how your enrollment status, doctor's certification, and homebound status all connect to determine eligibility.
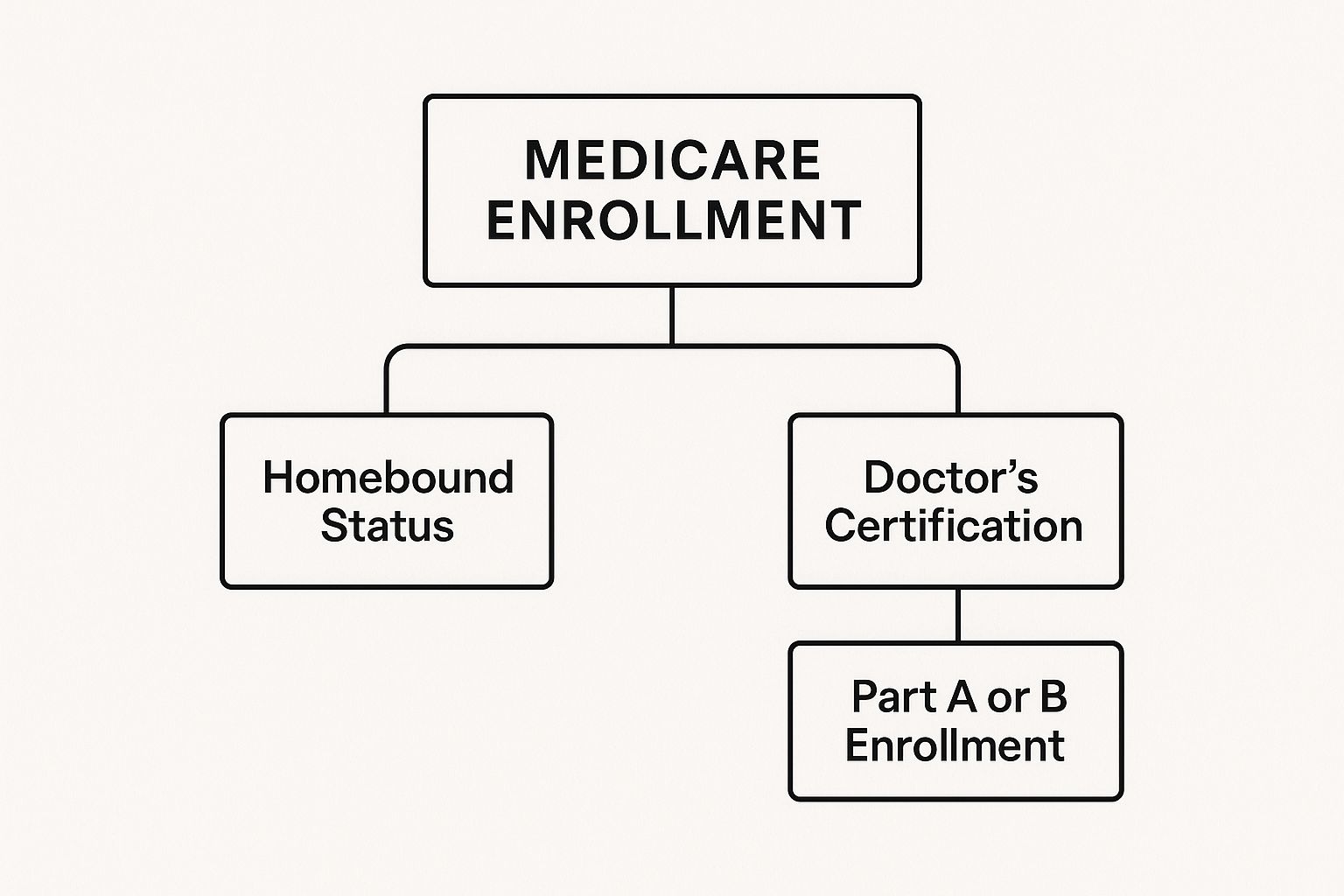
The image clearly shows that the doctor's certification and your homebound status are two critical pillars supporting your approval, highlighting their equal importance in the process.
Gate 3: Defining "Homebound" Status
The term "homebound" is probably the most misunderstood requirement of all. It does not mean you are bedridden or can never leave your house. Instead, Medicare's definition has two parts:
- Leaving your home takes a considerable and taxing effort because of an illness or injury.
- You can still leave home for medical appointments or for short, infrequent outings like attending a religious service, a family event, or getting a haircut.
For example, a patient recovering from major surgery might find a trip to the grocery store completely exhausting, even if they can manage their physical therapy appointments. This person would likely be considered homebound. The key is communicating with your doctor so your condition is documented accurately.
Gate 4: Medicare Part A and/or Part B Enrollment
Finally, you must be enrolled in either Medicare Part A (Hospital Insurance), Part B (Medical Insurance), or both. For approved home health services, Medicare typically covers 100% of the cost. There is no deductible or coinsurance for the services themselves.
However, it's important to remember that you are still responsible for a 20% coinsurance payment for any durable medical equipment (DME), such as a walker or hospital bed, that is ordered as part of your care plan. Once you've passed through these four gates, you can access the care you need to recover safely in the comfort of your own home.
Complete Service Menu: From Nursing to Medical Equipment
Once you qualify for Medicare home health benefits, you gain access to a wide range of services designed to help you recover right in the comfort of your own home. Think of this not as an à la carte menu, but as a coordinated toolkit. Just like a mechanic uses specific tools to repair an engine, your home health agency combines different services to build a care plan that’s tailored specifically for you.

This plan is centered around the need for skilled, intermittent care, which is the foundation of your benefits. These aren't simple custodial services; they are medical treatments delivered by licensed professionals who bring their expertise to you.
Skilled Nursing and Therapy Services
The heart of home health care is the skilled services that require a trained professional’s touch. These are the treatments that are central to your recovery and form the core of your plan of care.
- Skilled Nursing Care: This is the most frequently used service. Nurses do far more than just check your blood pressure. They manage complex medication schedules, administer IV drugs, provide catheter care, and perform advanced wound care. For patients with serious injuries, this professional oversight is crucial. You can learn more about how to heal deep wounds faster with this kind of expert care in our detailed guide.
- Physical Therapy (PT): After surgery, an illness, or an accident, a physical therapist helps you get back on your feet. They design personalized exercise programs that use your own home environment to help you safely climb stairs, get in and out of bed, and regain your independence.
- Occupational Therapy (OT): While PT is about restoring movement, OT is about restoring your ability to perform daily activities. An occupational therapist might help rearrange your kitchen to make cooking safer or teach you new techniques for dressing yourself when mobility is limited.
- Speech-Language Pathology Services: Also known as speech therapy, these services are for patients who have trouble speaking, swallowing, or communicating, often due to a stroke or another neurological condition.
Medical Social Services and Home Health Aides
While skilled care is the key to unlocking your benefits, Medicare also covers other support services when they are part of a care plan that includes nursing or therapy. These services address your wider well-being.
Medical social workers act as a bridge, connecting you and your family with vital community resources like meal delivery programs, transportation options, or support groups. They help you manage the emotional and social hurdles that often come with a significant health challenge.
Home health aides assist with personal care, such as bathing, dressing, and grooming. It’s important to understand that you can only receive aide services if you are also getting skilled nursing or therapy. Medicare will not cover aide services by themselves.
Durable Medical Equipment (DME) and Supplies
A vital component of your Medicare home health benefits is coverage for necessary medical equipment and supplies. While the home health services are typically covered at 100%, you are usually responsible for a 20% coinsurance for most durable medical equipment (DME).
Medicare helps pay for items your doctor orders for use at home, including:
- Hospital beds
- Walkers and wheelchairs
- Oxygen equipment
- Wound care supplies (like dressings and cleansers)
- Catheters
The home health agency handles the ordering and delivery of these supplies, making sure you have everything you need for a safe and effective recovery at home. This integrated approach ensures all parts of your care—from hands-on therapy to essential equipment—work together seamlessly.
To help you understand what's covered and how often, here is a detailed breakdown of the services available under Medicare's home health benefit.
Medicare Home Health Covered Services and Frequency Limits
Detailed breakdown of each service type, coverage criteria, and visit limitations under Medicare home health benefits
| Service Type | Coverage Criteria | Frequency Limits | Patient Cost Share | Common Uses |
|---|---|---|---|---|
| Skilled Nursing Care | Must be medically necessary and ordered by a doctor. | Intermittent or part-time (less than 8 hours/day and fewer than 7 days/week). | $0 (covered at 100%) | Wound care, IV therapy, injections, medication management, patient education. |
| Physical Therapy (PT) | Must be a specific, safe, and effective treatment for the patient's condition. | Medically necessary visits as determined by the therapist and doctor. | $0 (covered at 100%) | Restoring mobility after surgery, stroke, or injury; strength training; gait and balance training. |
| Occupational Therapy (OT) | Aims to improve the ability to perform daily activities (e.g., eating, dressing). | Medically necessary visits as determined by the therapist and doctor. | $0 (covered at 100%) | Adapting home environments, learning to use adaptive equipment, regaining fine motor skills. |
| Speech-Language Pathology | Addresses communication or swallowing disorders. | Medically necessary visits as determined by the therapist and doctor. | $0 (covered at 100%) | Recovering speech after a stroke, treating swallowing problems (dysphagia). |
| Home Health Aide | Can only be provided alongside skilled nursing or therapy services. | Part-time or intermittent. Cannot be the sole reason for home health care. | $0 (covered at 100%) | Assistance with personal care like bathing, dressing, and grooming. |
| Medical Social Services | Must be ordered by a doctor to address social/emotional issues related to illness. | Intermittent, as needed to resolve specific issues. | $0 (covered at 100%) | Counseling, connecting to community resources (e.g., Meals on Wheels). |
| Durable Medical Equipment (DME) | Must be prescribed by a doctor for home use and be long-lasting. | Varies by item. | 20% coinsurance after meeting the Part B deductible. | Hospital beds, walkers, wheelchairs, oxygen equipment. |
| Medical Supplies | Must be used to treat the illness or injury (e.g., wound dressings, catheters). | As needed for care provided by the agency. | $0 (covered at 100%) | Wound dressings, catheter supplies, irrigation solutions. |
This table shows how each service fits into the Medicare home health framework. While most hands-on care and supplies are fully covered, it's important to remember the 20% coinsurance for durable medical equipment. This comprehensive benefit package is designed to provide all the necessary tools for a successful recovery at home.
Understanding Costs: What You Actually Pay
One of the most attractive parts of Medicare home health benefits is the cost. For patients who qualify, the core skilled services—like professional nursing care and physical therapy—are typically covered at 100%. This means you won’t face a deductible or coinsurance for the main services provided by the home health agency. For families needing medical support at home, this is a significant relief.
However, it's a common mistake to think these benefits are entirely "free." The main exception to the $0 cost-sharing rule is for durable medical equipment (DME). If your care plan requires a hospital bed, a walker, or an oxygen machine, you'll generally be responsible for 20% of the Medicare-approved amount after you meet your annual Part B deductible. While the home health agency helps arrange for this equipment, the billing falls under a different part of your Medicare coverage.
Navigating Payment Changes and Potential Gaps
The financial side of home health care is also influenced by broader government policies. To ensure care is both high-quality and affordable, payment models are often updated. For example, for Calendar Year (CY) 2025, the Centers for Medicare & Medicaid Services (CMS) finalized a 0.5% payment increase for home health agencies, which injects about $85 million into the system. These adjustments are designed to align payments with patient needs rather than the number of visits. You can review the details of the CY 2025 home health payment system directly on the official CMS website.
These behind-the-scenes financial changes can affect which agencies offer certain specialized programs or how they bundle services. It's also important to know what Medicare does not cover. These non-covered services include:
- 24-hour care at home
- Meal delivery
- Homemaker services (such as cleaning or shopping)
- Custodial care (assistance with daily activities like bathing or dressing, if this is the only care you need)
For patients who need this kind of non-medical help or want to cover the 20% DME coinsurance, a Medigap (Medicare Supplement Insurance) policy can be a great help. These plans are sold by private companies to fill the "gaps" in Original Medicare, creating a more predictable budget. For families dealing with long-term recovery, like those needing extensive at-home wound care, a Medigap policy often provides crucial peace of mind. By planning for these potential out-of-pocket costs, you can keep your focus where it belongs: on healing.
Application Process: From Doctor's Order To First Visit

Starting the process for Medicare home health benefits is a bit like following a recipe. It starts with a key ingredient—your doctor's order—and moves through selecting your care team to the first official visit at home. Every step must be completed correctly to ensure your care begins smoothly. The official green light for your benefits is the order from your physician.
Your role in this first step is more important than you might think. When you talk with your doctor, be an active partner in the conversation. Clearly describe why leaving your home is a major physical challenge. Instead of just saying "it's hard to get out," give specific examples, like feeling completely drained after a short walk or needing help just to make it to an appointment. This detail helps your doctor build a solid case in your medical records, which is precisely what Medicare looks for.
Choosing Your Home Health Agency
After your doctor sends the order, you get to decide which Medicare-certified home health agency will provide your care. While your doctor’s office might suggest a few local agencies, the choice is ultimately yours. This is a significant decision, as this group of professionals will be your partners in recovery.
Treat the selection process like you're hiring someone for an important job. When you call potential agencies, have a list of questions ready:
- What is your patient-to-nurse ratio? A lower number often translates to more one-on-one attention.
- How do you manage questions or emergencies after normal business hours? You want to be sure a reliable support system is available 24/7.
- Can you tell me about your experience with my specific condition? If you have a serious wound, for example, you should ask about their specific wound care expertise. Learning about pressure ulcer treatment in home care can give you an idea of the specialized skills needed.
- How will you communicate and coordinate with my main doctor? Strong communication between your care team and physician is vital for effective treatment.
Listen carefully to how the agency staff answers. A good provider will be transparent, patient, and happy to address your concerns. Be wary of vague responses, any pressure to decide quickly, or an unwillingness to provide references.
The Intake Process and Your First Visit
Once you've picked an agency, they will arrange an initial intake assessment. A registered nurse will come to your home to perform a detailed evaluation. This isn't just a simple check-in; this assessment is used to create your official plan of care. The nurse will review your medical needs, check your home for safety, and talk with you about your personal goals for recovery.
This first visit is your chance to build a solid foundation with your care team. You can prepare by making sure walkways are clear and there's a well-lit space for the nurse to work. Have your list of medications and any questions you've thought of ready to go. If family members will be helping with your care, it’s a good idea for them to be there too. This meeting helps turn your home into a safe and supportive space for healing.
Complex Medical Needs: Wound Care And Advanced Services
For patients managing serious health challenges—like chronic wounds from diabetes, recovery after surgery, or major mobility issues—the standard medicare home health benefits become an essential support system. This is where care goes far beyond simple check-ins and becomes high-level medical treatment delivered in your own home. Receiving advanced care at home isn't just about convenience; it’s about creating a better, more focused environment for healing.

Advanced Wound Care at Home
Think about the difficulty of managing a severe, non-healing wound that used to mean weekly trips to a special clinic or even a hospital stay. With Medicare home health, skilled nursing teams bring that same level of clinical care directly to you. These nurses are trained to manage complex treatments that are crucial for preventing infection and helping tissue repair.
This includes advanced procedures such as:
- Negative Pressure Wound Therapy (NPWT): Often called a "wound vac," this technology uses a special vacuum-assisted device. It gently draws fluid away from the wound, which helps reduce swelling and encourages the growth of new, healthy tissue.
- Complex Dressing Changes: This is much more than putting on a new bandage. Nurses use specialized dressings, medicated ointments, and debridement techniques (the careful removal of dead tissue) to create the ideal conditions for healing.
- Infection Management: Home health nurses are trained to spot the early signs of infection. They can take cultures for testing and even administer IV antibiotics right at home, helping you avoid a trip back to the hospital.
This in-home model is especially effective because healing is a unique journey for every person. The close teamwork between your home health nurse and dedicated wound care specialists ensures your treatment plan is constantly adjusted based on your progress. Excellent home health wound care patient outcomes are often the direct result of this personalized and consistent attention.
Rehabilitation for Complicated Conditions
Beyond wound care, therapists also adjust their approaches for patients with significant health obstacles. Imagine a physical therapist working with a patient who has both severe arthritis and a heart condition. Instead of assigning generic exercises, the therapist would create a gentle, low-impact program that builds strength without straining the heart or joints.
In another example, an occupational therapist could help a stroke survivor with limited mobility relearn how to cook safely in their own kitchen. The therapist might suggest adaptive tools or help rearrange the kitchen to lower the risk of falls, giving the patient the power to reclaim a sense of independence and daily routine. This is rehabilitation that meets you where you are, working within the real-world limits of an illness or disability.
A Case Study in Recovery
Let's look at the story of a patient recovering from major abdominal surgery. Sent home from the hospital while still weak and with a complex incision, this person would typically face frequent and uncomfortable trips to the surgeon's office.
With Medicare home health benefits, a skilled nurse visited daily for the first week to manage the surgical wound, monitor for infection, and make sure pain was under control. A physical therapist designed a gentle walking plan using the patient's own hallway, slowly increasing the distance. At the same time, an occupational therapist helped them practice getting in and out of bed safely.
In just a few weeks, the patient wasn't only healing physically but had also rebuilt the confidence to manage their recovery at home, all while following hospital-level safety measures. This is the power of bringing expert, complex care into the home.
Maximizing Your Medicare Home Health Benefits
Getting approved for Medicare home health benefits is a fantastic step forward in your recovery, but it’s only the beginning. The real magic happens when you actively manage your care and become a true partner with your health professionals. Think of your home health team—your nurses, therapists, and aides—as your personal support crew. The better you work together, the smoother your journey to better health will be. Making the most of these benefits comes down to open communication, smart coordination, and understanding your role in the process.
Building a Strong Partnership with Your Care Team
A positive relationship with your home health team is the bedrock of successful care. This starts with getting ready for each visit. Before your nurse or therapist arrives, take a moment to consider how you've been feeling. It's helpful to jot down any new symptoms, questions, or challenges you've encountered since their last visit. This simple preparation makes your time together focused and productive.
Good communication flows in both directions. Be honest about how you're doing, even if progress feels slow. If an exercise is causing too much pain or a new medication has side effects, speak up right away. Your team can only adjust your care plan if they have a complete picture of what's going on. Addressing small issues early can prevent them from becoming bigger problems later.
To help this partnership thrive, try these strategies:
- Keep a Simple Log: A dedicated notebook for your home health care can be a powerful tool. Use it to track your good and bad days, list questions as they pop into your head, and note any instructions from your care team.
- Designate a Point Person: If you have several family members involved, choosing one person to be the main contact helps prevent confusion. This ensures clear and consistent communication with the agency.
- Ask for Clarification: If you don't understand a medical term or an instruction, ask your nurse or therapist to explain it in a different way. It’s your health, and you have every right to understand all aspects of your care.
Coordinating Care and Tracking Progress
Your home health team is just one piece of your overall healthcare puzzle. It's essential to make sure they are in sync with your primary doctor and any other specialists you visit. When your home health nurse suggests a change, confirm that this information is shared with your doctor. This creates a seamless care experience and prevents risky gaps in treatment, which is especially important for complex needs like wound management.
Systematically tracking your own progress is also vital. This isn't just for your own motivation; it provides the documented evidence needed to justify continued coverage if your condition requires care for a longer period. For instance, if you're getting physical therapy, you could track how many more steps you can walk each week or if you can stand for longer periods. This data clearly shows the medical necessity and effectiveness of your Medicare home health benefits.
Transitioning and Understanding Your Rights
Ultimately, the aim of home health care is to help you "graduate"—either back to living independently or, if needed, to a different level of care. A good home health agency will begin planning this transition with you from day one. They will help you set realistic goals and make sure you have the skills and support needed to manage safely on your own.
As a patient, you have specific rights regarding the quality of your services. If you ever feel your care isn't meeting professional standards, you have the right to voice your concerns. Your first step should be to speak with the agency's clinical supervisor. If that doesn't fix the problem, you can contact your state's survey agency or the Beneficiary and Family Centered Care-Quality Improvement Organization (BFCC-QIO). Being an active, informed participant ensures you get the full value from your care.
For those managing complicated wounds, getting the right specialized care is crucial. Rapid Wound Care brings expert wound management directly to your home, working within your existing Medicare benefits to provide treatments that speed up healing. Learn how our at-home wound specialists can support your recovery today.

