Why Proper Wound Assessment Changes Everything
Accurate wound assessment is the cornerstone of effective wound care. It's not just a routine step; it's the crucial first step in creating a successful treatment plan and ensuring the best possible healing. This thorough evaluation establishes a baseline for tracking progress, allowing healthcare professionals to adjust treatment as needed.
For example, a wound that initially seems minor might reveal underlying issues upon closer examination. Early detection, through a comprehensive assessment, can prevent small problems from becoming serious complications.
The Impact of Accurate Assessment
Thorough wound assessment helps prevent a series of negative outcomes that can significantly impact a patient's well-being and healthcare expenses. Without a clear understanding of the wound's characteristics, healthcare providers might choose ineffective treatments, delaying healing and prolonging suffering.
Inaccurate assessments can also contribute to complications such as infections, which often require hospital readmissions and longer hospital stays. These setbacks increase healthcare costs and diminish the patient's quality of life.
Furthermore, wound assessment is crucial because of its significant impact on healthcare systems. In the United States, chronic wound care costs an estimated $28 billion each year, demonstrating the financial burden these conditions place on healthcare providers. Globally, chronic wounds affect over 40 million people, severely impacting their quality of life. Learn more about the global impact of wounds here. This highlights the critical need for accurate and timely wound assessment as a vital part of effective healthcare strategies.
The Role of Technology in Wound Assessment
Technology is changing the way we assess wounds, improving precision and objectivity. It's like upgrading from a basic ruler to a high-resolution digital camera; the detail and accuracy are significantly enhanced. New tools, such as digital imaging and AI-powered analysis, provide detailed measurements and identify subtle changes that might be missed by the naked eye.
This allows for earlier intervention and more personalized treatment plans. Healthcare professionals can track healing progress more effectively and use data to make informed decisions to improve patient outcomes.
Essential Elements Every Assessment Must Include
Wound assessment is a crucial process that goes beyond simply checking off boxes. It's a systematic approach guiding effective treatment by helping clinicians spot subtle infection signs, accurately measure wound dimensions, and evaluate overall wound health. These carefully assessed parameters can predict healing success or alert clinicians to potential complications. This meticulous method ensures consistent evaluations, regardless of a clinician's experience.
Key Wound Characteristics to Observe
Assessing a wound involves observing specific characteristics, much like piecing together a puzzle. Each observation contributes to a comprehensive understanding of the wound's status. These characteristics are fundamental for effective wound assessment.
-
Location: Pinpointing the wound's anatomical location helps understand potential causes and influences treatment strategies.
-
Size: Precisely measuring the wound's length, width, and depth creates a baseline for monitoring healing progress. Want more information about different wound types? Check out this resource: How to master the assessment of various wound types.
-
Tissue Type: Evaluating the tissue type within the wound bed (granulation, slough, eschar) provides insights into the healing phase and guides debridement needs.
-
Exudate: Assessing the amount, color, and consistency of wound drainage helps determine the appropriate dressing and identifies potential infection.
-
Periwound Skin: Examining the surrounding skin for maceration, erythema, or edema helps assess the wound's impact on nearby tissues.
Wound Irrigation Volumes
Effective wound cleaning through irrigation is essential for healing. The amount of irrigation solution needed depends on the wound size. The infographic below illustrates recommended irrigation volumes for different wound sizes.
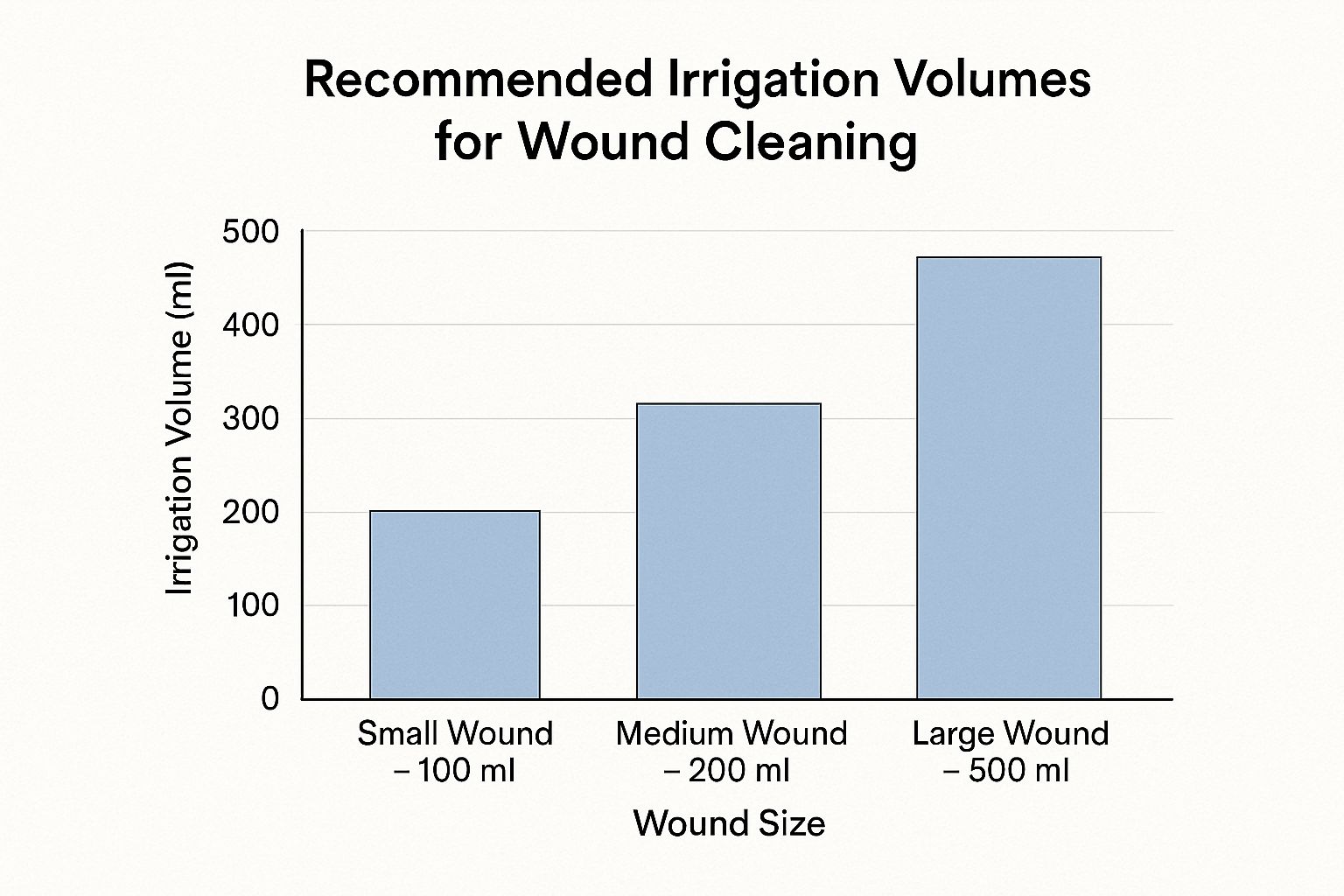
As the infographic shows, a small wound typically requires 100 ml of irrigation solution. A medium wound needs 200 ml, and a large wound requires 500 ml. Using the correct volume ensures thorough cleaning without harming delicate wound tissue. Proper irrigation, combined with accurate assessment, is vital for preventing infection and promoting healing.
The following table summarizes key wound assessment parameters and what constitutes normal healing versus concerning findings, along with the appropriate action to take.
Wound Assessment Parameters and Normal vs. Concerning Findings
| Assessment Parameter | Normal/Healing Signs | Concerning Findings | Action Required |
|---|---|---|---|
| Location | Clearly defined edges | Spreading redness or swelling beyond wound margins | Monitor closely, consider culture if infection suspected |
| Size | Gradual reduction in size | Increasing size, deepening | Re-evaluate treatment plan, consider advanced therapies |
| Tissue Type | Healthy granulation tissue (pink/red, moist) | Necrotic tissue (black eschar, yellow slough), excessive fibrous tissue | Debridement as needed, consider topical treatments |
| Exudate | Moderate amount, clear or serosanguinous | Large amount, purulent, foul odor | Culture for infection, adjust dressings, consider antimicrobial therapy |
| Periwound Skin | Intact, normal color and temperature | Maceration, erythema, edema, warmth | Address moisture balance, protect surrounding skin, consider topical barrier cream |
This table provides a quick reference guide for clinicians conducting wound assessments. Recognizing these signs early can significantly impact patient outcomes.
Documenting Your Findings
Clear and concise documentation is essential for effective wound management. It's like keeping a detailed log of the wound's progress, providing valuable information for other healthcare professionals and ensuring continuity of care. Documentation helps determine treatment protocols, evaluate their effectiveness, and provide context for future assessments. It also allows for tracking progress over time. This documentation should include all key wound assessment elements to provide a complete record of the wound's condition and response to treatment.
This systematic approach to wound assessment ensures every evaluation captures crucial details, leading to informed treatment decisions and improved patient outcomes. It also improves communication among healthcare providers, fostering a collaborative approach to wound care.
Your Step-by-Step Assessment Process That Actually Works

This section offers a practical, step-by-step guide for assessing wounds effectively. Whether you're dealing with a simple surgical incision or a complex chronic ulcer, this process uses best practices from experienced clinicians to ensure comprehensive and accurate evaluations.
Preparing For The Assessment
Creating the right environment is the first step in a thorough wound assessment. This includes gathering the necessary supplies, ensuring adequate lighting, and positioning the patient comfortably for both their well-being and clear visibility of the wound. Proper preparation allows for a more focused assessment.
-
Gather Supplies: Assemble everything you'll need. This includes a ruler or measuring tape, sterile cotton swabs, gloves, a good light source, and your documentation tools.
-
Ensure Proper Lighting: Accurate visual assessment requires good lighting. Use a direct light source to clearly illuminate the wound and the surrounding tissue.
-
Position the Patient: Make sure the patient is comfortable to minimize their discomfort during the assessment. Their position should also allow you easy access to the wound.
Conducting The Wound Assessment
Once you've prepared your environment and gathered your supplies, you can begin the systematic examination of the wound and the surrounding area. This involves measuring the wound, evaluating the tissue, and noting any signs of infection. A careful, meticulous approach ensures that you don't overlook any important details.
-
Measure the Wound: Precisely measure the wound's length, width, and depth using a ruler or measuring tape. For irregularly shaped wounds, use the clock method for consistency. Record the dimensions in centimeters.
-
Evaluate the Tissue: Assess the wound bed for tissue type (granulation, slough, eschar) and note the color and condition of the surrounding skin. Look for signs of maceration, erythema, or edema.
-
Assess for Infection: Check for any indicators of infection. This includes purulent drainage, a foul odor, increased pain, or redness and swelling around the wound.
-
Document Undermining and Tunneling: If undermining or tunneling are present, use a cotton swab to measure and document their extent. Describe their location using the clock method for clarity.
Patient Involvement and Next Steps
Patient education and involvement are critical components of the assessment process. Engaging the patient empowers them to participate in their healing and improves communication with healthcare providers. This approach also ensures continuity of care.
-
Involve the Patient: Explain the assessment process to the patient, addressing any questions they may have. Encourage them to actively participate in monitoring their wound and reporting any changes.
-
Determine Next Steps: Based on your assessment findings, determine the appropriate treatment plan. This may include dressing selection, debridement needs, and referrals to specialists. You might also find helpful information on deep wound healing: How to master deep wound healing.
-
Document Findings: Clearly document all your findings, including measurements, tissue descriptions, signs of infection, and planned interventions. Use standardized medical terminology for clear communication among healthcare professionals.
This detailed process ensures a thorough wound assessment, leading to accurate diagnosis, effective treatment planning, and improved patient outcomes. By following these steps, healthcare professionals can confidently assess wounds and contribute to better patient care.
Advanced Techniques That Elevate Your Practice

Building on established methods, wound care is evolving with new assessment tools. These tools promise more accurate and consistent wound evaluations. From digital imaging to AI-powered analysis and smartphone apps, these technologies offer exciting ways to improve wound assessment.
Digital Imaging and AI: A New Era of Assessment
Digital imaging provides a high-resolution look at wounds, capturing details often missed by the human eye. AI-powered software can analyze these images, identifying subtle shifts in wound characteristics and even predicting healing progress. This gives clinicians valuable insights into the wound's condition.
For example, some AI platforms can measure wound area with incredible precision, minimizing the inconsistencies of manual measurements. This technology also allows for objective assessment of tissue types, pinpointing problem areas and guiding treatment choices.
Smartphone Apps: Bringing Assessment to the Point of Care
Smartphone apps make wound assessment more portable and convenient. These apps can capture images, measure wounds, and track healing over time. This allows both clinicians and patients to monitor wounds effectively.
Some apps even include telehealth features, enabling remote consultations for wound care, particularly useful in areas with limited resources. This expands access to specialized wound care expertise.
The Growing Market for Wound Healing Assessment
The wound healing assessment market is projected to grow significantly, reaching $161.8 million by 2032. This growth is fueled by technological advancements and an aging population, representing a 5.2% CAGR from 2025. You can find detailed statistics here.
Integrating New Tools Into Your Workflow
Adopting these advanced techniques requires careful planning. While powerful, these tools should enhance, not replace, clinical judgment. Healthcare professionals need proper training to use them effectively.
Cost can be a barrier to adopting new technology. However, many institutions find the long-term benefits of improved accuracy and fewer complications outweigh the initial investment. These advancements hold great promise for improving wound assessment and management.
Adapting Assessment Across Different Care Settings
Assessing a wound in a busy hospital is very different from assessing one in a patient's home. While the fundamental principles remain consistent, adjusting your techniques to each individual environment is essential for accurate evaluation. This adaptability is a key characteristic of effective healthcare professionals, enabling them to deliver high-quality care regardless of the location.
Acute Care vs. Home Health: Tailoring Your Approach
In an acute care setting, you typically have access to advanced tools, optimal lighting, and a controlled environment. In contrast, home health settings may have limited resources, suboptimal lighting, and challenges with patient mobility.
This means you may have to adjust your assessment process while still including the key elements: accurate measurement, tissue evaluation, and checking for infection. For instance, if specialized measuring tools are unavailable, you could use a standard ruler and the "clock method" to record wound dimensions.
Additionally, family members are often actively involved in home healthcare. Teaching them how to assess a wound and spot any worrying changes between professional visits becomes extremely important.
Overcoming Challenges in Home Settings
Home assessments come with their own unique hurdles. Poor lighting can make it hard to accurately assess tissue type and notice subtle signs of infection. Limited mobility equipment can also make proper positioning for a comprehensive examination difficult.
To overcome these obstacles, consider bringing a portable light source to improve visibility. If the patient has limited mobility, get creative with positioning—perhaps using pillows or blankets for support. You might be interested in: How to master effective post-discharge wound care at home. The growth of home healthcare has increased the need for skilled nurse visits for wound care. Data reveals that wounds result in higher skilled nurse visit utilization at 16.7 visits per stay compared to 7.0 for all clinical groups in 2022. Learn more about this trend here.
Empowering Family Caregivers
Family caregivers are vital partners in home wound care. Teach them the basics of wound assessment, emphasizing what looks normal and what might indicate a problem. Clear instructions on checking for changes in size, drainage, or the surrounding skin can help prevent complications.
Regular communication with the healthcare team is also crucial. Encourage caregivers to document their observations and contact a professional if they see anything concerning. Empowered caregivers play a significant role in positive patient outcomes at home. This collaborative method fills the gap between professional visits, ensuring consistent monitoring and timely intervention. It also promotes a more patient-centered approach, improving the overall quality of care.

Documentation That Makes a Difference
A thorough wound assessment relies heavily on the quality of its supporting documentation. Clear and concise records effectively communicate the wound's status among healthcare professionals, ensuring everyone is well-informed. This shared understanding is essential for making sound decisions and providing consistent care. It also contributes valuable data for quality improvement analysis.
Why Detailed Documentation Matters
Accurate documentation is more than just a formality; it directly affects patient well-being. It creates a clear timeline of the wound's progression, enabling healthcare providers to understand its history, track its progress, and anticipate potential issues. This detailed history promotes better collaboration and smoother transitions of care, especially when multiple providers are involved.
Meticulous documentation also plays a vital role in clinical decision-making. A comprehensive overview of the wound informs treatment choices, allowing for more personalized care and improving the likelihood of successful healing. Furthermore, proper documentation fulfills regulatory requirements and protects healthcare providers by demonstrating the standard of care provided.
Essential Elements of Effective Documentation
Effective documentation captures all the essential assessment details in a clear and accessible manner. This balance of comprehensiveness and clarity ensures the information is both informative and practical, providing a clear narrative of the wound's progress.
-
Wound Location: Use precise anatomical terms to document the wound's location, preventing confusion and ensuring accurate communication.
-
Measurements: Record accurate measurements of the wound's length, width, and depth. For irregular wounds, use the clock method for consistent measurement. Document any undermining or tunneling.
-
Tissue Description: Describe the appearance of the wound bed (granulation, slough, eschar) and surrounding skin. Note the color, texture, and any signs of infection.
-
Exudate Characteristics: Record the amount, color, odor, and consistency of wound drainage to inform dressing selection.
-
Pain Assessment: Use a standardized pain scale to document the patient's pain level, enabling effective pain management and tracking.
-
Photographs: Include photographs with a ruler for scale. This creates a visual record of the wound, improving communication among healthcare professionals. Read also: How to master wet-to-dry dressing changes.
To better understand the necessary documentation, refer to the table below:
Introducing the following table, "Essential Documentation Elements for Comprehensive Wound Assessment," outlines the key components required for thorough wound documentation, providing examples and explaining their clinical significance.
| Documentation Element | Required Details | Example Entry | Clinical Significance |
|---|---|---|---|
| Wound Location | Precise anatomical location | "2 cm superior to the lateral malleolus, left lower extremity" | Ensures accurate communication and targeted treatment |
| Measurements | Length, width, depth, undermining, tunneling | "Length: 4.5 cm, Width: 3 cm, Depth: 1.5 cm, Undermining: 1 cm at 12 o'clock" | Tracks wound size and progression |
| Tissue Description | Wound bed and periwound skin characteristics (color, texture, signs of infection) | "Wound bed: 100% granulation tissue, beefy red; Periwound skin: intact, pink, warm" | Indicates healing status and potential complications |
| Exudate Characteristics | Amount, color, odor, consistency | "Moderate serosanguineous drainage" | Guides dressing selection and infection monitoring |
| Pain Assessment | Patient's pain level using a standardized scale | "Pain: 3/10 on the numerical rating scale" | Informs pain management strategies and monitors effectiveness |
| Photographs | Images with a ruler for scale | Photo with ruler included | Provides visual record and enhances communication |
This table highlights the crucial aspects of wound documentation, emphasizing the importance of detailed and accurate recording for effective wound management.
Optimizing Your Documentation Process
Efficient documentation doesn't require sacrificing detail; it's about working smarter. Electronic health records (EHRs) can significantly reduce paperwork, improve efficiency, and enhance accuracy.
By optimizing EHR templates and using standardized terminology, you can create concise yet comprehensive records that save time and improve communication across disciplines. This increased efficiency allows you to dedicate more time to patient care, ultimately enhancing the quality of care provided.
Overcoming Real-World Assessment Challenges
Wound assessment is more than just textbook knowledge. Real-world scenarios often present unique complexities that can challenge even experienced healthcare professionals. This section explores common, yet difficult, situations encountered in wound assessment.
Difficult Anatomical Locations
Assessing wounds in areas like the groin, buttocks, or under pendulous breasts presents logistical challenges. These locations often involve awkward positioning for both the patient and clinician, along with limited visibility. Maintaining patient privacy and dignity is also crucial. The solution lies in adaptability and prioritizing patient comfort. Use pillows to support the patient and improve positioning. Consider alternative lighting sources or magnifying tools to enhance visibility.
Patient Discomfort
Assessing some wounds can be inherently painful. Patients with burns, deep ulcers, or sensitive skin may experience considerable discomfort during examinations. This can make a thorough assessment difficult. To mitigate pain, consider pre-medicating the patient as appropriate. Always use gentle handling techniques. Ensure the wound bed is adequately moistened before any manipulation. Clearly explain each step of the process to the patient to empower them and give them a sense of control.
Heavily Exudating Wounds
Excessive exudate can obscure the wound bed, making it challenging to assess underlying tissue. Understanding the wound bed’s condition is paramount for effective treatment planning. Managing exudate is key. Use highly absorbent dressings to control excess fluid. Consider advanced wound care therapies, such as negative pressure wound therapy (NPWT), to manage exudate and improve visualization.
Edema and Tissue Viability
Edema can mask the true extent of tissue damage, making it difficult to accurately assess tissue viability. The swelling obscures the underlying tissue, potentially misrepresenting its health. Differentiating viable from non-viable tissue becomes challenging, potentially impacting treatment decisions. Serial assessments are helpful to monitor changes over time. Consult with a wound care specialist for advanced diagnostics like laser Doppler flowmetry to assess blood flow and tissue perfusion.
External Pressures
External pressures from colleagues, family members, or even patients can sometimes influence clinical judgment. These pressures can affect the objectivity of wound assessment data interpretation. Maintaining objectivity is crucial for unbiased decision-making. This necessitates clear communication and meticulous documentation of findings. Explain your assessment process and rationale to all parties, emphasizing the importance of evidence-based care.
Managing Complex Presentations
Not all wounds fit neatly into defined categories. Some present with unusual characteristics or a combination of factors complicating assessment. These complex wounds require a multi-faceted approach. For example, a diabetic foot ulcer with heavy exudate and surrounding edema presents multiple assessment challenges. Consider the resource: How to master treating diabetic foot ulcers. In these cases, consulting with experienced wound care specialists is invaluable.
By developing strategies to navigate these real-world challenges, you can gain confidence in assessing any wound, regardless of complexity. This expertise results in more informed decisions, better patient outcomes, and increased job satisfaction.
Ready to experience specialized wound care? Rapid Wound Care provides comprehensive at-home wound care services, offering personalized treatment plans for various wound conditions. Visit Rapid Wound Care today to learn more and schedule a consultation.

