The Evolution of Healing: NPWT Through the Ages
Negative pressure wound therapy (NPWT) might appear to be a recent medical innovation, but its origins go back much further than you might think. Understanding its historical journey provides valuable context for how this therapy works and its impact on modern wound care. This evolution showcases how basic concepts, refined over centuries, transformed into the sophisticated technology used today.
The earliest versions of NPWT date back to the 19th century with the use of basic cupping techniques. While rudimentary, these techniques offered early glimpses into the potential of negative pressure to promote healing. They established the foundation for more complex applications in the future, inspiring physicians to explore the therapeutic power of suction for wound treatment.
From Glass Leeches to Cupping Systems: Early Innovations
In 1821, Dr. Francis Fox introduced the "Glass Leech," a suction device created to simulate the then-prevalent practice of leech therapy. This innovative tool, a wide-necked cup designed to adhere to the skin, represented a significant advancement in applying negative pressure to wounds. Later, in 1890, Dr. Gustav Bier expanded on this idea with a more versatile cupping system. His system utilized glass cups of varying sizes and shapes, connected by tubing to a bulb, enabling the extraction of fluids from wounds across multiple body areas. These early advancements set the stage for the more sophisticated NPWT devices used in contemporary medicine. Learn more about the evolution of NPWT.
From Battlefield to Hospital: Wartime Advancements
The 20th century saw substantial progress in NPWT, largely spurred by the demands of wartime medicine. During the Soviet-Afghan conflict, Soviet surgeon Dr. Nail Bagaoutdinov encountered the challenge of treating infected wounds in austere environments. In 1985, he began combining negative pressure units with foam dressings, marking a pivotal moment in the development of NPWT. This wartime innovation proved remarkably effective, highlighting the therapy's potential even under the most challenging conditions.
The Birth of Modern NPWT: Polyurethane Foam and Vacuum Systems
Building on these wartime discoveries, the modern era of NPWT began in the early 1990s. Drs. Louis Argenta and Michael Morykwas at Wake Forest University pioneered the use of polyurethane foam with mechanical vacuum systems, further refining the technology. Their work propelled NPWT from a niche technique to a widely accepted and highly effective treatment for a broad spectrum of wounds. This marked the beginning of widespread clinical use of negative pressure wound therapy as we recognize it today.
Continued Advancement: Digital Monitoring and Specialized Interfaces
The evolution of NPWT continues to this day. Current systems offer advanced digital monitoring capabilities, customizable settings, and specialized wound interfaces. These technological improvements have enhanced the effectiveness of NPWT and broadened its applications, establishing its critical role in modern wound care. The journey from simple cupping to advanced digital systems demonstrates the transformative power of medical innovation in wound healing.
The Science Behind How Negative Pressure Wound Therapy Works
Negative pressure wound therapy (NPWT) has changed wound care. But how does it work? NPWT combines physics and biology to create an environment that helps the body heal, both visibly and at a microscopic level.
Understanding the Basics of Negative Pressure
NPWT uses controlled negative pressure (a vacuum) at the wound site. This vacuum does more than remove unwanted materials; it starts a chain reaction of helpful effects. It removes extra wound exudate and infectious material, which lessens edema (swelling from fluid buildup). This, in turn, improves blood flow and oxygenation, vital for cell repair. NPWT also causes macrostrain (the wound contracting from the foam) and microstrain (microscopic cell stretching). Microstrain encourages cell growth, angiogenesis (new blood vessel growth), and the development of granulation tissue, all essential for healing.
NPWT has been linked to quicker wound closure and shorter hospital stays, lowering costs and improving patient results. NPWT with instillation (NPWTi-d) takes this further by automatically delivering topical solutions, offering better control and wound management. These developments have made NPWT useful for more complex wounds worldwide. Learn more here.
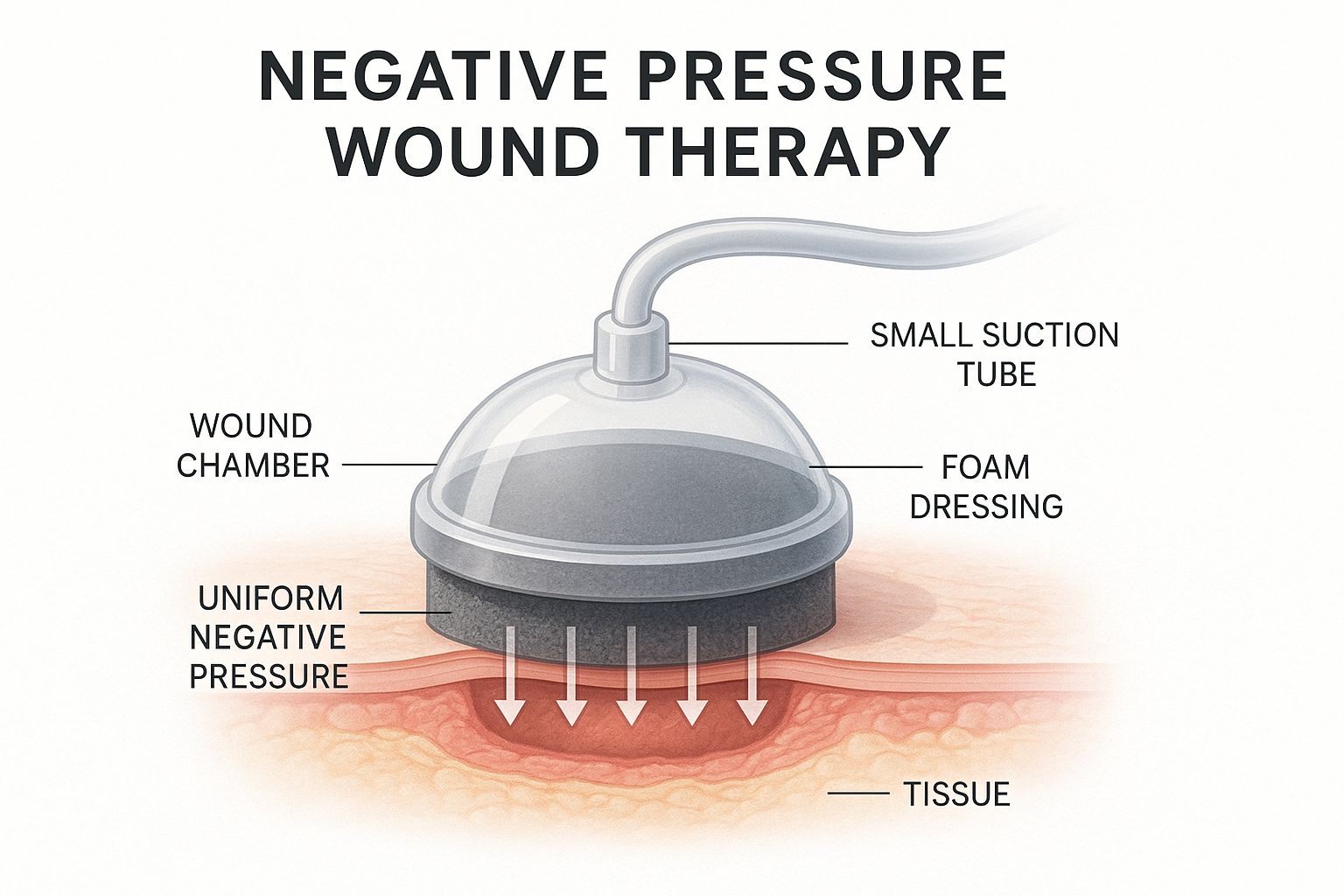
This infographic illustrates a wound chamber connected to a suction tube, with foam dressing applying negative pressure to the tissue.
The foam dressing evenly distributes negative pressure across the wound. This even pressure and fluid removal create an ideal healing environment. Understanding the history of wound care can be helpful; for instance, the evolution of home care shows the ongoing effort to improve healing. You may also find this resource helpful: How to heal deep wounds faster.
The Cellular Level: Microstrain and Angiogenesis
Besides removing fluids, NPWT impacts cells. Microstrain, the tiny stretching of cells, boosts cell growth and new blood vessel formation (angiogenesis). Angiogenesis brings oxygen and nutrients to the wound, speeding up healing. This microscopic activity is just as important as the visible fluid removal.
Macrostrain and Wound Contraction
Negative pressure also creates macrostrain, a force that pulls the wound edges together. This shrinking reduces the wound's size, helping it close faster. It's like tightening a drawstring bag; the edges are gently pulled together. This complements the microscopic effects of NPWT.
Maintaining a Moist Healing Environment
NPWT also keeps the wound moist. A special dressing seals the wound, preventing it from drying out and protecting it from outside germs. Moisture is essential for cell growth and tissue repair. It's like a tiny greenhouse for the wound.
To further illustrate the benefits of NPWT, let's examine the physiological effects:
| Mechanism | Effect on Wound | Clinical Benefit |
|---|---|---|
| Removal of exudate | Reduces excess fluid and bacteria | Decreases infection risk, improves healing environment |
| Reduced edema | Less swelling | Improves blood flow and oxygenation |
| Macrostrain | Wound contraction | Faster wound closure |
| Microstrain | Cellular stretching | Promotes cell growth and angiogenesis |
| Moist environment | Prevents wound desiccation | Facilitates tissue regeneration |
This table summarizes the key ways NPWT promotes healing. The combined effects of fluid management, mechanical forces, and maintaining a moist environment contribute to improved patient outcomes.
Modern NPWT Technologies: Evolution of Healing Systems
Negative pressure wound therapy (NPWT) has evolved significantly over the years. Originally, bulky equipment limited its use to hospitals. Now, portable NPWT systems integrate seamlessly into a patient's daily life. This transformation is a result of continuous advancements by biomedical engineers and wound care specialists.
From Basic Pumps to Intelligent Systems: A Technological Leap
Early NPWT devices relied on simple mechanical vacuum pumps and standard foam dressings. Today's systems offer digital monitoring, customizable settings, and specialized wound interfaces. These features provide clinicians with greater control over therapy and allow for personalized treatment. Imagine the difference between a basic on/off switch and a computer that monitors and adjusts settings in real time. That level of precision is now a reality with modern NPWT.

Modern NPWT systems are portable and user-friendly.
Instillation Therapy: A Game-Changer in Wound Care
One of the most significant advancements in NPWT is instillation therapy. This technique combines negative pressure with the application of wound cleansing solutions directly to the wound bed. It's similar to a power washer for wounds, gently cleansing and promoting healing at the same time. This combination provides a more thorough approach to wound management. Instillation therapy has expanded the use of NPWT for challenging wound types. You can learn more about post-discharge wound care at home here.
Expanding the Scope of NPWT: Addressing Diverse Needs
Since the first commercial NPWT systems appeared nearly three decades ago, countless innovations have broadened their application across healthcare. Early devices had limitations. Now, we have a wider array of dressing interfaces, tubing designs, power sources, and even canister-free options. Integrated wound solution instillation, smart monitoring technology, and various disposable and reusable units have also been developed. These advancements now allow clinicians to treat wounds in patients previously unsuitable for NPWT, such as those with highly exudative or complex wounds. The increased versatility and safety have led to wider adoption of these devices in the United States, Europe, and Asia. NPWT is regularly used for chronic wounds, acute surgical wounds, traumatic injuries, and diabetic foot ulcers, establishing it as a multi-billion dollar global market. Further explore this topic here.
To better understand the evolution of NPWT, let's take a look at the following table:
Evolution of NPWT Systems: Comparison of features between early and modern NPWT devices
| Feature | Early NPWT Systems | Modern NPWT Systems | Clinical Advantage |
|---|---|---|---|
| Portability | Limited | Portable/Canister-Free options | Increased patient mobility and comfort |
| Pressure Control | Basic | Digital/Customizable settings | Precise pressure delivery and monitoring |
| Instillation | Not available | Integrated instillation | Enhanced wound cleansing and medication delivery |
| Dressings | Limited options | Wide range of specialized dressings | Tailored to specific wound types |
| Monitoring | Basic | Smart monitoring/Data logging | Improved wound assessment and treatment optimization |
This table highlights the key differences between early and modern NPWT systems. The advancements in portability, pressure control, instillation, dressings, and monitoring have significantly improved the efficacy and patient experience of NPWT.
Selecting the Right System: A Personalized Approach
With numerous options available, selecting the right NPWT system is essential. Important factors include the wound type, the patient’s lifestyle, and their specific clinical needs. For instance, a portable, canister-free system might be ideal for an active person. A system with instillation therapy may be more appropriate for a complex wound. This personalized approach is key for maximizing the effectiveness of NPWT and enhancing patient outcomes.
Finding Your Match: Which Wounds Benefit Most From NPWT
Negative pressure wound therapy (NPWT) offers distinct advantages in wound care. However, it's not a one-size-fits-all solution. Knowing which wounds respond best is crucial for effective treatment. This involves careful evaluation of the wound's characteristics and the patient's overall health. Let's explore which wounds often improve with NPWT and when other treatments might be better. Learn more in our article about the different types of wounds.
Chronic Wounds: A Strong Case for NPWT
Chronic wounds, such as diabetic foot ulcers, pressure injuries (bedsores), and venous ulcers, frequently benefit from NPWT. These wounds are typically slow to heal and susceptible to infection. NPWT helps by removing excess fluid, promoting blood flow, and encouraging tissue growth. This creates an environment that promotes healing. Diabetic foot ulcers, especially, often show marked improvement.
Acute Wounds: Assessing the Benefits
NPWT can be helpful for some acute wounds like surgical incisions and traumatic wounds. However, it's not always the primary treatment. Deciding to use NPWT for acute wounds often depends on factors like the wound's depth, size, and location. For instance, a deep surgical wound with a high infection risk might benefit from NPWT. A superficial wound might heal well with standard dressings.
Traumatic Wounds and Burns: NPWT Considerations
NPWT can be utilized in managing traumatic and burn wounds. Its use depends on factors like the degree of tissue damage, infection presence, and the patient’s overall health. NPWT assists by managing exudate, minimizing swelling, and prepping the wound bed for potential skin grafting. However, NPWT might not be recommended with significant dead tissue present, which may require debridement or surgery.
Other Wound Types and NPWT
- Dehisced surgical wounds: NPWT can facilitate closure and reduce infection risk in reopened surgical wounds.
- Open abdominal wounds: In complex abdominal wounds, NPWT can manage exudate and safeguard exposed tissues.
When NPWT Might Not Be Suitable: Contraindications
While NPWT is useful for many wound types, some situations make it inappropriate. Untreated osteomyelitis (bone infection), necrotic tissue with eschar (dead tissue with a hard covering), and untreated fistulas (abnormal connections between organs or tissues) are generally contraindications for NPWT. Addressing these underlying issues before starting NPWT is critical. Cancer in the wound is also a contraindication.
Wound Assessment: Guiding Treatment Decisions
Thorough wound assessment is crucial in determining if NPWT is appropriate. Factors like wound depth, size, location, exudate amount, infection presence, and overall patient health all influence the decision. A comprehensive evaluation by a wound care specialist is essential for safe and effective treatment. This assessment determines NPWT suitability and guides the selection of appropriate settings and dressings.
The Patient Journey: Living With Your NPWT System

Starting negative pressure wound therapy (NPWT) can be a new experience. This section offers a realistic look at what patients can expect, addressing common questions and providing helpful tips for daily life with an NPWT system. Understanding both the mechanics of NPWT and the personal experience is crucial.
What to Expect During Treatment
Your first appointment will include a thorough wound assessment and a discussion of the NPWT process. The clinician will explain how the device works, answer your questions, and ease any concerns. This initial meeting is important for establishing open communication with your healthcare team.
Once therapy starts, you'll feel the vacuum. Most patients describe it as a gentle pulling, not usually painful. The device might make a low hum, but newer models are designed to be quieter. These initial sensations often lessen over time.
Managing Daily Life with NPWT
Many patients wonder how NPWT will affect their daily routines. Showering is usually possible with a waterproof dressing or by temporarily disconnecting the device (always consult your clinician first). You can adjust your sleeping position with the device; most patients find comfortable positions that minimize disruption. You may need to adapt some daily activities, but many individuals can maintain a relatively normal life.
- Showering: Use waterproof dressings or talk to your clinician about disconnecting the device temporarily.
- Sleeping: Try different positions to find what’s most comfortable for you.
- Daily Activities: Adjust tasks as needed, but try to maintain your usual routine.
You might be interested in this resource on post-discharge wound care: How to master post-discharge wound care.
Recognizing Potential Complications and Seeking Support
While NPWT is generally safe, it’s important to know the potential complications. Increased pain, bleeding, or any signs of infection should be reported to your clinician immediately. Regular follow-up appointments are vital for checking progress and addressing any issues. Remember, you have support throughout this process.
Emotional Well-being and Quality of Life
Living with a wound can be emotionally difficult. Talking with your healthcare team, support groups, or loved ones can help. Staying positive and doing things you enjoy can greatly improve your quality of life during treatment. For more information, visit Rapid Wound Care.
Practical Tips for Managing Your NPWT System
- Keep the dressing clean and dry: This helps prevent infection and allows the device to function properly.
- Follow your clinician’s instructions carefully: This includes dressing changes and vacuum settings, personalized for your specific needs.
- Communicate openly with your healthcare team: Don't hesitate to ask questions or discuss any concerns. They are there to support you.
Measuring Success: Real Results From Negative Pressure
Negative pressure wound therapy (NPWT) has created a lot of buzz in the wound care field. But how effective is it in practice? This section explores the tangible results of NPWT, focusing on what matters most to both patients and healthcare professionals. We'll delve into clinical studies to understand NPWT's impact on healing time, infection rates, and quality of life across various wound types.
Key Indicators of Effective NPWT
Several factors point to the effectiveness of NPWT. A healthy wound bed will visibly show more granulation tissue, a pinkish, fleshy tissue indicating healing. Decreased wound size and depth are also positive signs. Less exudate (fluid drainage) usually suggests the wound is healing. Beyond what's visible, biomarkers can provide more detailed insights into the healing process. These markers reflect the cellular and molecular activity within the wound, offering a more complete picture of the therapy's effectiveness. Keeping a well-stocked first aid kit on hand is always a good idea for managing minor wound-related issues.
Realistic Timeframes and Expectations
While individual healing times differ, studies suggest NPWT can often speed up wound closure. Some research shows a 22% reduction in healing time for certain wound types. It's important to have realistic expectations, however. Chronic wounds, such as diabetic foot ulcers, may still require several weeks or even months to heal fully, even with NPWT. Regular checkups with a wound care specialist are essential to track progress and adjust treatment accordingly. For more information on this specific type of wound, you can learn more about treating diabetic foot ulcers.
Cost-Effectiveness Compared to Traditional Methods
NPWT can often be more cost-effective than traditional wound care methods over time. The initial investment in NPWT equipment might seem higher, but reduced hospital stays, fewer complications, and quicker healing can result in lower overall costs. For instance, by reducing the need for frequent dressing changes, NPWT saves both time and resources. Preventing infections and other complications with NPWT also helps avoid costly additional treatments.
Tracking and Documenting NPWT Progress: Best Practices
Clinicians utilize several methods to monitor and document NPWT progress. Regular photographic documentation creates a visual record of the wound's healing over time. Measuring wound size and depth is also crucial for tracking progress. Additionally, patient-reported outcomes, including pain levels and quality of life, are increasingly important indicators of treatment success. Clinicians may also use specialized software to manage and analyze wound data, enabling a more precise and personalized approach to care. This data-driven method ensures that NPWT is used effectively, maximizing patient outcomes and optimizing resource use.
Are you or someone you care for dealing with a non-healing wound? Rapid Wound Care provides comprehensive at-home wound care services, including negative pressure wound therapy. Our team of certified professionals is dedicated to providing personalized care to help you achieve optimal healing. Visit our website today to learn more and schedule a consultation.

