The Science Behind Effective Home Health Wound Care
Effective wound care is a science. Understanding the fundamentals of home health care is essential. Wound healing isn't as simple as applying a bandage. It's a complex biological process with distinct phases.
These phases—inflammation, proliferation, and maturation—work together to repair damaged tissue. During the initial inflammatory phase, the body sends white blood cells to the wound to fight infection and remove debris. This first step is crucial for proper healing. Understanding these stages allows for appropriate care at each point in the process.
The home environment also plays a vital role in healing. Factors like room temperature and humidity significantly impact how a wound closes and resists infection. A wound needs the right conditions to thrive. Just as a plant needs sunlight and water, a wound needs a balanced environment to heal efficiently. Even pets can introduce bacteria, emphasizing the need for a clean environment. For more information, check out this article on how to heal deep wounds faster.
Factors That Influence Wound Healing at Home
Many home environmental factors can affect healing speed. Maintaining optimal humidity, for example, prevents wounds from drying out and forming scabs, which can slow tissue regeneration. This can be achieved with humidifiers or proper ventilation.
A comfortable room temperature promotes good blood circulation to the wound, delivering nutrients and oxygen. This is like providing fertilizer for a plant. Proper temperature avoids extremes that constrict blood vessels and hinder healing.
Minimizing irritants like dust, pet dander, and harsh chemicals is also crucial. These can cause inflammation and prolong healing. By managing the home environment, you create ideal conditions for natural healing.
The Growing Need for Home Health Wound Care
The importance of home health wound care is highlighted by the growing global demand. The market is expanding steadily, driven partly by demographics. Projections for 2025 anticipate a CAGR of approximately 5-6%, continuing a recent trend.
This growth is linked to the aging global population. By 2030, the World Health Organization estimates 1 in 6 people will be aged 60 or older. This represents an increase from 1 billion older adults in 2020 to 1.4 billion in 2030. Older adults often need wound care for surgical wounds and chronic issues like diabetic ulcers.
The United States represents over 45% of global wound care product consumption and more than half the overall market volume. However, emerging economies like China, India, and Singapore are seeing the fastest growth in demand. This global increase requires advancements in technology and innovation to address challenges like personnel shortages and supply chain issues, shaping the future of home health wound care. You can read more about the future of wound care. This surging demand emphasizes the need for accessible and effective home health wound care solutions, allowing individuals to manage their healing comfortably at home.
Creating Your Home Wound Care Arsenal
Building a practical home wound care kit doesn't require a medical degree or breaking the bank. It's about having the right tools, not every gadget available. This guide, drawing on advice from experienced home health nurses, helps you build a cost-effective and efficient system.
Essential Supplies: Separating Needs From Wants
Begin by gathering the core items for your wound care kit. This includes sterile dressings, like gauze pads and non-stick bandages, to protect the wound and absorb fluids. Antiseptic solutions, such as saline or hydrogen peroxide, are crucial for cleaning the wound. Medical tape and bandages secure dressings. Having these readily available simplifies the care process, much like having basic ingredients in your kitchen.
Additionally, consider versatile items that offer good value. Non-latex gloves protect both you and the patient from infection. Disposable scissors prevent cross-contamination. A small plastic container is useful for soaking or cleaning. These enhance efficiency without adding unnecessary expense.
Organization and Sterility: Maintaining an Efficient System
Organized storage is crucial once you have your supplies. A designated, clean area for your wound care kit, like a drawer, shelf, or plastic bin, maintains sterility. Organize logically, grouping similar items for easy access during dressing changes. This saves time and creates a calm, efficient care environment.
Maintaining sterility is paramount. While you don't need a hospital setup, basic hygiene is vital. Always wash your hands thoroughly before and after dressing changes. Use clean surfaces and avoid touching the wound directly. Regularly check expiration dates on supplies and replace expired items promptly. These simple practices significantly reduce infection risk and encourage healing.
Managing Costs and Insurance: Practical Considerations
Home wound care can be budget-friendly. Compare prices at different pharmacies and consider buying in bulk for frequently used items. Ask your doctor about reusable supplies to reduce waste. Many insurance plans, including Medicare, cover some home wound care supplies. Understanding your coverage can minimize out-of-pocket costs. Planning your purchases, like budgeting for groceries, saves money without sacrificing quality.
To help you compare essential wound care supplies, we've created a handy table outlining their uses, benefits, drawbacks, and approximate costs.
Introducing the "Essential Home Wound Care Supplies Comparison" table, designed to guide you in choosing the right supplies for your needs:
| Supply Type | Best For | Advantages | Limitations | Approximate Cost Range |
|---|---|---|---|---|
| Gauze Pads | Absorbing drainage, packing wounds | Highly absorbent, versatile, cost-effective | Can stick to the wound, requires frequent changes | $2 – $10 per box |
| Non-Stick Bandages | Minor cuts, abrasions | Protects the wound, minimizes pain during dressing changes | Not suitable for heavily draining wounds | $3 – $8 per box |
| Saline Solution | Cleaning wounds, irrigating | Gentle, non-irritating, readily available | May not be effective against all bacteria | $5 – $15 per bottle |
| Hydrogen Peroxide | Disinfecting wounds | Strong antiseptic properties | Can damage healthy tissue if used excessively | $1 – $5 per bottle |
| Medical Tape | Securing dressings | Strong adhesive, various sizes available | Can irritate sensitive skin | $2 – $7 per roll |
| Hydrocolloid Dressings | Minor burns, blisters, pressure sores | Promotes moist wound healing, protects from friction | Not suitable for infected wounds | $10 – $30 per box |
| Alginate Dressings | Moderate to heavily draining wounds | Highly absorbent, promotes healing | Can dry out the wound if not properly managed | $15 – $40 per box |
By reviewing this table, you can better understand the various supplies available and make informed decisions about which ones best suit your particular wound care requirements. Remember to consult with your healthcare provider for personalized recommendations.

The traditional wound care market, encompassing bandages, gauze, and dressings, is a significant segment within home health wound care. This market is projected to reach USD 9.12 billion by 2030, growing at a CAGR of 4.2% from its USD 7.42 billion value in 2025. This growth is fueled by the increasing prevalence of chronic conditions and a growing elderly population, increasing the need for wound care at home. Find more statistics here.
By following these tips, you can create a well-stocked and efficient home wound care setup for effective healing and minimized costs.
Mastering Wound Cleaning Techniques That Actually Work

Proper wound cleaning is essential for effective home health wound care. It's more than just basic first aid; it involves specific techniques that significantly improve healing. This section explores professional methods for ensuring optimal wound recovery. Learn more in our article about effective post-discharge wound care at home.
The Art of Gentle Yet Effective Cleaning
Cleaning a wound effectively means removing debris without harming the delicate healing tissue. Imagine dusting a fragile antique – you want to remove the dirt without damaging the surface. Gentle, precise movements are key.
First, wash your hands thoroughly and put on gloves. Then, irrigate the wound with a sterile saline solution. This washes away loose debris and bacteria. Avoid harsh scrubbing, which can damage new tissue and slow down healing.
Instead, use gentle, outward strokes starting from the center of the wound. This directs debris away from the healing area. Pat the wound dry with sterile gauze, avoiding any rubbing. The right technique creates a clean environment that supports optimal healing.
Adapting Techniques for Different Locations
Where a wound is located significantly affects how you should clean it. A wound on a flat surface like the forearm requires a different approach than one in a crevice, such as behind the knee. Adaptability is crucial.
For hard-to-reach areas, consider using tools like cotton swabs or syringes with angled tips. These tools allow precise application of cleaning solutions without disturbing the wound.
Patient comfort during the procedure is also important. Use pillows or other supports to help access the wound while minimizing discomfort. Proper positioning ensures thorough cleaning and patient comfort.
Pain-Free Dressing Changes: A Key to Healing
Changing dressings can be uncomfortable. Minimizing pain promotes healing and reduces stress. The correct technique makes a big difference.
Before removing the old dressing, gently loosen the adhesive. If it's stuck, moisten it with saline solution. This minimizes pain and pulling on the wound. Remove the dressing slowly and smoothly, pulling in the direction of hair growth to reduce discomfort.
When applying a new dressing, make sure it's the correct size and material for the wound. Secure it gently, avoiding excessive pressure, which can restrict blood flow. A properly applied dressing promotes both healing and comfort.
Common Mistakes and Practical Workarounds
Even with the best intentions, mistakes can happen. One common error is using tap water to clean wounds. Tap water, although convenient, may contain microorganisms that can interfere with healing. Using sterile solutions like saline is essential.
Another mistake is aggressively cleaning the wound. While it might seem logical to scrub away debris, this actually damages fragile new tissue. Gentle irrigation and cleaning are much more effective.
For individuals with limited mobility, adaptive equipment like long-handled sponges or dressing applicators can be helpful. These tools allow individuals to maintain their independence and ensure proper wound care.
Patient and Caregiver Insights: Real-World Advice
Learning from those with experience in home wound care offers valuable insights. Many caregivers recommend establishing a regular routine for dressing changes. This minimizes stress and ensures consistent care.
Patients often suggest having all the necessary supplies organized and readily available before beginning a dressing change. This streamlines the process, making it more efficient and comfortable.
By mastering these techniques and incorporating advice from experienced patients and caregivers, you can confidently manage home health wound care, leading to better healing and an improved quality of life.
Customizing Care for Different Wound Types
Not all wounds are the same. Just as different plants thrive under specific conditions, different wound types require unique approaches in home health wound care. Understanding these nuances is essential for effective healing. This means recognizing the distinct characteristics of common wound types and adapting care strategies accordingly.
Common Wound Types and Their Characteristics
Diabetic ulcers, frequently found on the feet, are a common complication of diabetes resulting from poor circulation and nerve damage. These wounds often appear as deep, slow-healing sores and require meticulous care to prevent infection. Pressure injuries, also known as bedsores, develop from prolonged pressure on the skin, usually over bony areas. These wounds necessitate frequent repositioning and specialized dressings to alleviate pressure and encourage blood flow. Learn more in this article about the six types of wounds.
Surgical wounds, created during surgical procedures, require careful monitoring for signs of infection. Keeping the area clean and dry is crucial. Vascular ulcers, arising from poor blood circulation in the legs, are characterized by irregular edges and slow healing. Compression therapy is often a necessary part of their management.
Tailoring Treatment to the Wound
The underlying cause of a wound significantly impacts its treatment. For instance, a diabetic ulcer requires careful blood sugar management in addition to local wound care. This comprehensive approach addresses the root cause while promoting healing. A pressure injury, on the other hand, needs frequent repositioning and pressure-relieving surfaces. This minimizes further damage and allows the wound to heal.
Wound location also plays a vital role in treatment strategies. A wound near a joint needs flexible dressings that allow for movement without disrupting the healing process. A wound on a less mobile area may benefit from a more rigid dressing for added protection. This adaptability ensures the treatment supports the body's natural healing process.
The infographic below visualizes key data related to wound healing and home care: it compares average healing times for minor and moderate wounds, shows dressing change frequency, and illustrates the impact of proper home care on infection risk reduction.
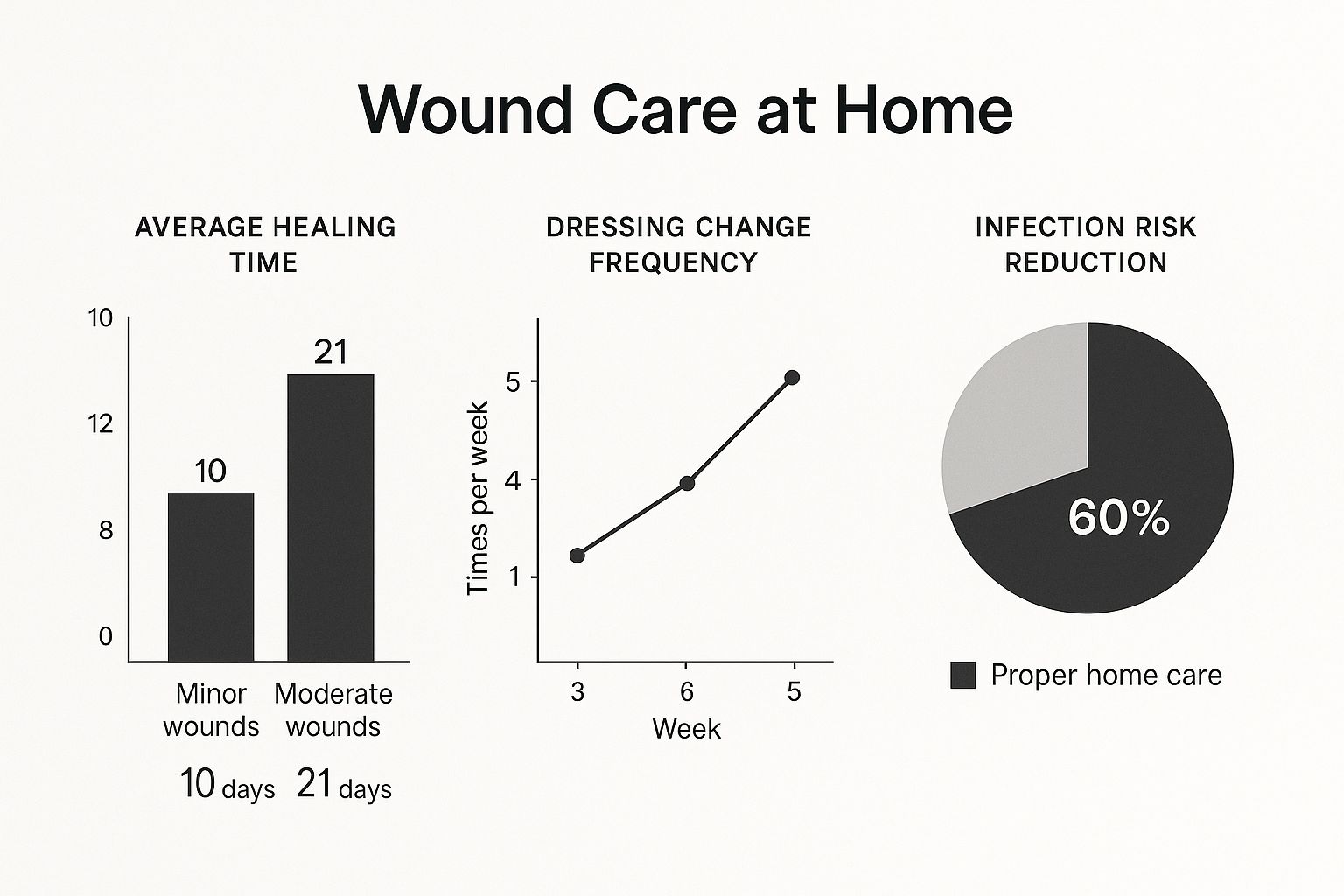
As the infographic shows, minor wounds heal much faster than moderate wounds, requiring fewer dressing changes per week. Proper home care dramatically reduces the risk of infection, highlighting the importance of diligent home health wound care practices.
Advanced Wound Care and Market Growth
Advanced wound care, incorporating treatments like collagen therapy and negative pressure wound therapy, addresses chronic wounds resistant to conventional methods. This market is projected to grow from USD 11.82 billion in 2025 to approximately USD 18.04 billion by 2034. This expansion is fueled by the increasing prevalence of chronic wounds, especially diabetic foot ulcers, which affect 15-25% of individuals with long-standing diabetes. Learn more about advanced wound care.
Recognizing Healing and Identifying Complications
Knowing when a wound is healing properly is essential for successful home health wound care. Positive healing signs include a decrease in wound size, the formation of healthy granulation tissue (new, pink tissue), and reduced pain and swelling. This progress indicates that the body’s natural healing processes are working effectively.
Sometimes, interventions are necessary. Signs like increased pain, swelling, redness, foul odor, or excessive drainage can indicate infection. Changes in wound color, like darkening or blackening of the tissue, might signal poor circulation. Recognizing these warning signs allows for timely intervention and prevents further complications. This careful observation is crucial in home health wound care to ensure optimal healing and avoid complications.
The following table provides further guidance on specific wound types, their characteristics, and recommended care approaches:
Wound Types and Recommended Care Approaches
| Wound Type | Key Characteristics | Recommended Dressings | Changing Frequency | Warning Signs |
|---|---|---|---|---|
| Diabetic Ulcer | Deep, slow-healing, often on feet | Non-adherent, absorbent dressings | As directed by physician, often daily | Increased pain, swelling, redness, foul odor |
| Pressure Injury | Shallow or deep, over bony prominences | Pressure-relieving dressings, foam, hydrocolloids | Varies based on wound stage and dressing type | Darkening tissue, foul odor, increased drainage |
| Surgical Wound | Incision site, may have sutures or staples | Sterile gauze, transparent films | As directed by physician, usually every 1-3 days | Redness, swelling, pus, fever |
| Vascular Ulcer | Irregular edges, slow-healing, often on legs | Compression bandages, absorbent dressings | Daily or as directed by physician | Increased pain, swelling, discoloration, leg cramps |
This table summarizes key aspects of wound care and provides a quick reference for identifying warning signs that require medical attention. Always consult with a healthcare professional for any concerns about wound healing.
The Healing Power of Nutrition in Wound Recovery
What you eat plays a vital role in home health wound care, just as important as how you dress a wound. This section explores the science behind nutritional healing, highlighting specific foods and nutrients that can significantly improve the speed of tissue repair.
The Building Blocks of Healing: Protein, Vitamins, and Minerals
Think of your body as a construction site, and a wound is like a damaged building. Protein is essential, acting like the bricks and mortar needed for rebuilding tissue. Without enough protein, wound healing can be significantly slowed down.
Vitamins and minerals, such as vitamin C and zinc, are like the construction workers, facilitating the biochemical processes involved in tissue repair. Vitamin C is crucial for collagen synthesis, building the framework of new tissue. Zinc supports cell growth and division. Without these essential nutrients, the body's repair crew cannot work efficiently.
Creating a Healing Diet: Practical Tips and Meal Plans
You might be interested in: How home wound care speeds up recovery. Creating a diet that promotes wound healing doesn’t need to be complex. Focus on including protein-rich foods like lean meats, poultry, fish, beans, and lentils. These provide the essential building blocks for tissue repair.
Be sure to get enough vitamins and minerals, too. Colorful fruits and vegetables are excellent sources. Dark leafy greens are packed with vitamin A, which is important for cell growth. Citrus fruits are full of vitamin C, essential for collagen production. Eating a variety of these foods ensures a balanced nutrient intake.
Addressing Challenges: Loss of Appetite and Dietary Restrictions
Loss of appetite is common during recovery. However, good nutrition is vital for healing. To address this, try eating smaller, more frequent meals throughout the day. This can be more manageable than large meals when your appetite is low.
Consider nutrient-dense smoothies or protein shakes for a convenient way to boost your nutrient intake. These provide a concentrated dose of nutrients in an easily digestible form. Dietary restrictions can present challenges, but working within them is crucial. A registered dietitian can help you create a meal plan that meets your specific needs.
Sample Meal Plans: Fueling Different Stages of Healing
Different wound types and stages of healing may benefit from different nutritional approaches. During the initial inflammatory phase, focus on antioxidant-rich foods to help reduce inflammation. Berries, for example, are high in antioxidants.
As the wound moves into the proliferative phase, prioritize protein and vitamin C to support tissue regeneration. Chicken breast with steamed broccoli is a great meal that combines these nutrients. In the final maturation phase, maintain a balanced diet emphasizing protein, vitamins, and minerals for scar formation and strengthening. A well-rounded diet throughout the entire healing process is key for a successful recovery.

Detecting Trouble Before It Becomes Serious
Effective home health wound care relies heavily on careful observation. Even small shifts in a wound's appearance can indicate important changes that require quick action. This section will empower you with the same observation skills professionals use, helping you spot early warning signs and prevent complications.
Recognizing Normal Healing vs. Warning Signs
Understanding the difference between typical healing and signs of trouble is essential. A healing wound may exhibit some clear fluid drainage, a thin layer of yellow or white film (fibrin), or slight redness around the edges. These are generally normal aspects of the healing process.
However, significant changes merit close attention. Thick, pus-like drainage, increased redness and warmth around the wound, a foul odor, or the appearance of red streaks extending from the wound are all red flags. These could point to an infection. A wound that stops shrinking, shows darkening tissue, or develops new, deep pockets may signal a problem with blood flow or the healing process itself.
Subtle Indicators of Infection: Catching It Early
Infections can escalate rapidly in a home health setting, making early detection crucial. Even before noticeable symptoms like fever or chills manifest, subtle cues can suggest a developing infection.
These indicators can include increased pain or tenderness at the wound site. Changes in drainage – becoming thicker, cloudy, or developing a foul smell – are also important to note. Unusual warmth or swelling around the wound, or even a slight shift in the wound's color towards a dusky or grayish tone, can also signal an early infection. Recognizing these subtle signs allows for prompt treatment.
Prevention Strategies: Minimizing Complication Risks
Preventing complications is paramount in home health wound care. Proper nutrition plays a key role in supporting the body's healing processes. Consider exploring natural inflammation remedies. Consistent and proper cleaning techniques, using sterile solutions and applying gentle pressure, significantly lower the risk of infection.
Keeping the wound appropriately dressed creates a protective barrier against contamination and promotes a moist healing environment. Additionally, avoiding smoking improves circulation, contributing to faster healing. These preventative measures work together to create a strong defense against potential issues.
Effective Monitoring and Documentation: Staying Organized
A systematic approach to monitoring simplifies home health wound care. Regularly photographing the wound allows you to visually track its progress over time. Maintaining a logbook with entries noting the date, time, and observations about the wound’s appearance, drainage, and the surrounding skin is also helpful.
This documentation provides a valuable record for both you and your healthcare providers. It helps identify patterns, evaluate treatment effectiveness, and support informed decisions about future care.
Communicating with Healthcare Providers: Clear and Concise Reporting
Open communication with your healthcare provider is essential. Describe any observed changes accurately and thoroughly. Sharing your wound logbook and photographs during appointments provides valuable context.
Don’t hesitate to ask questions or express any concerns. Clear communication ensures you receive appropriate guidance and support. This collaborative approach optimizes your home health wound care and ensures you receive personalized advice and prompt intervention if needed, ultimately promoting successful healing.
When to Call in Professional Home Health Wound Care
Knowing when to seek professional help for home health wound care is crucial, just as understanding basic wound care is. This section outlines the key indicators that signal the need for professional intervention, based on expert advice from wound care specialists.
Recognizing Signs That Require Professional Attention
While some changes are a normal part of the healing process, others indicate potential problems requiring professional home health wound care. A healthy wound typically shows gradual improvement. This includes reduced size, the formation of new pink tissue (granulation tissue), and decreased pain. For more information on a specific type of wound, you might be interested in: Learn more about treating diabetic foot ulcers.
However, certain changes warrant immediate attention. Increased pain, swelling, and redness around the wound, along with thick, pus-like drainage or a foul odor, could point to an infection. Red streaks extending from the wound are a particularly serious sign. If the wound stops getting smaller, darkens in color, or develops new, deep areas, it could signal problems with blood circulation. These are all instances where professional home health wound care becomes essential.
Communicating Effectively With Healthcare Professionals
Clear and concise communication is vital when contacting a healthcare professional. Describe what you've observed in detail, including any changes in the wound's appearance, drainage, or the surrounding tissue. Be specific about when these changes started and how long they've been present. Also, mention any related symptoms like fever or chills. This detailed information helps healthcare professionals accurately understand the situation and determine the best course of action.
Keeping a record of your observations, such as photographs or a wound logbook, can be incredibly helpful. This visual and written documentation provides valuable context for healthcare professionals, allowing them to track the wound's progress over time. Such organized information contributes to a more accurate assessment and a personalized treatment plan.
Professional Resources Available for Home Support
Several professional home health wound care resources are available to provide support. Home health agencies offer skilled nursing care, which includes wound assessment, dressing changes, and pain management. Certified wound care specialists can provide advanced treatments and create comprehensive care plans.
Telehealth services, such as those offered through platforms like Teladoc, offer remote consultations and monitoring. This provides convenient access to expert advice. Understanding the available resources helps you make informed decisions and find the appropriate level of support. This can significantly improve the effectiveness of your home health wound care.
Preparing for a Professional Assessment and Continuing Care
Preparing for a professional assessment helps ensure a smooth and productive process. Gather all relevant medical information, including a list of current medications, any allergies, and a history of past wound care treatments. Prepare a list of questions or concerns you might have. This proactive approach helps you get the most out of the visit.
Between professional visits, consistent home care is crucial. Follow the prescribed treatment plan diligently, keeping the wound clean and dressed as instructed. Continue monitoring the wound for any changes, and promptly report those changes to your healthcare provider. This collaborative approach optimizes healing and minimizes the risk of complications, ensuring you receive the full benefits of professional home health wound care.
Don't let wound care become overwhelming. Rapid Wound Care offers comprehensive, at-home wound care services for chronic wounds, pressure injuries, diabetic ulcers, and more. Our certified professionals provide personalized treatment plans and advanced therapies in the comfort of your home. We accept insurance, including Medicare Part B. Visit Rapid Wound Care today to learn more and schedule a consultation.

