Making Sense of Evidence-Based Wound Care Basics
Think of evidence-based wound care like baking a cake. You wouldn't just throw ingredients together and hope for the best, would you? You'd follow a recipe, carefully measuring and combining ingredients in a specific order. Similarly, evidence-based wound care follows a proven recipe, grounded in research and best practices, to ensure the best possible outcomes. This approach replaces guesswork with a reliable, predictable path toward healing.
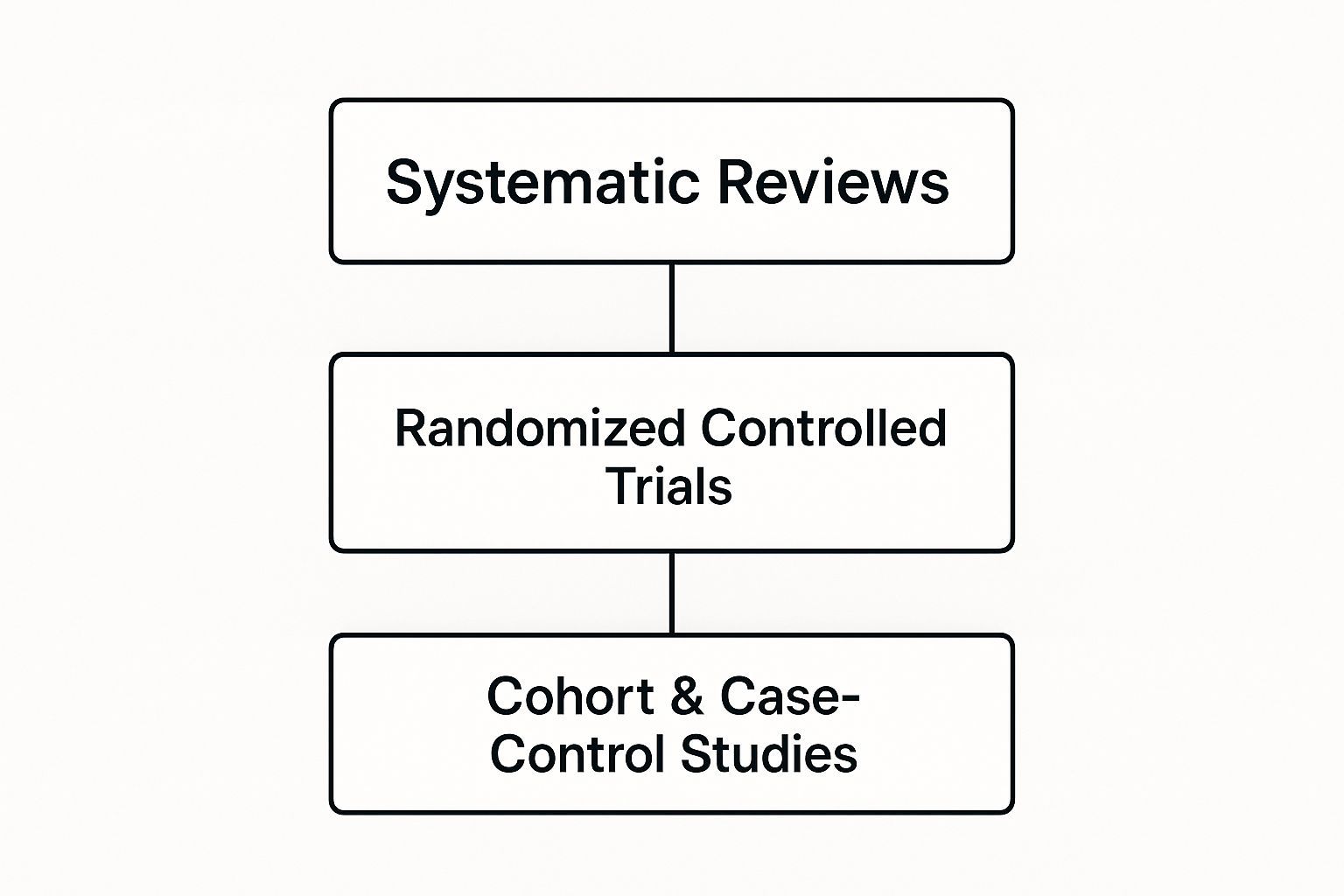
This infographic illustrates the hierarchy of evidence used in wound care. At the top, we have systematic reviews, which analyze data from multiple studies to provide the strongest evidence. Next, we have randomized controlled trials, followed by observational studies. This pyramid visually represents how healthcare professionals prioritize the most reliable research when making treatment decisions.
This data-driven approach is a major force behind the growth of the global wound care market. The market is expected to see a compound annual growth rate of 4.61% between 2023 and 2030, highlighting the increasing demand for effective wound care solutions. Learn more about these market trends in this study published by Mary Ann Liebert, Inc. publishers: Wound Repair and Regeneration.
Why This Shift Matters
Moving from intuition to evidence-based practice has dramatically improved patient care. This approach ensures consistent and reliable results, whether a patient is in a hospital or receiving care at home. Furthermore, it enables healthcare providers to anticipate and address potential problems proactively, shifting from a reactive to a preventative approach. For a deeper dive into wound care best practices, check out the Windy City Wound Care Knowledge Base.
Understanding the Core Principles
Evidence-based wound care stands on three fundamental pillars:
- Best Research Evidence: Treatment decisions are rooted in the most reliable scientific findings, not just tradition or personal preference.
- Clinical Expertise: Healthcare professionals combine this research with their own practical experience and professional judgment.
- Patient Values: Importantly, treatment plans take into account each patient’s unique needs, preferences, and circumstances.
This personalized approach ensures that care is not only effective but also tailored to each individual. For instance, treating a diabetic foot ulcer requires a different strategy than managing a surgical wound.
To further clarify the differences, let's examine the following table:
Traditional vs Evidence-Based Wound Care Approaches
This table compares traditional and evidence-based wound care methods, outcomes, and decision-making processes. It highlights the shift towards a more data-driven, patient-centered approach.
| Aspect | Traditional Approach | Evidence-Based Approach | Key Benefits |
|---|---|---|---|
| Decision-Making | Based on experience, anecdotal evidence | Driven by research, clinical guidelines | Standardized care, reduced variability in outcomes |
| Treatment Selection | Often trial-and-error | Targeted interventions based on evidence | More effective treatments, faster healing |
| Patient Involvement | Limited patient input | Shared decision-making with the patient | Improved patient satisfaction, adherence to treatment plans |
| Outcome Measurement | Subjective assessment | Objective data collection and analysis | Trackable progress, data-driven adjustments to treatment |
As you can see, evidence-based wound care offers numerous advantages over traditional methods.
The Impact on Patient Outcomes
By prioritizing scientific evidence, we see clear improvements in patient outcomes:
- Healing Rates: Wounds heal more quickly and efficiently.
- Reduced Infections: The chance of infection decreases significantly.
- Improved Quality of Life: Patients experience less pain and discomfort.
- Cost Savings: Effective care can minimize the need for costly procedures.
This focus on tangible results makes evidence-based wound care a crucial component of modern healthcare, leading to better care and improved outcomes for everyone.
How Research Actually Changes Healing Outcomes

Think of your body's healing process like renovating a house. You have demolition (clearing out damaged tissue), framing (building new connective tissue), and the final finishes (new skin). Each step needs to happen at the right time with the right tools. Evidence-based wound care is like the general contractor, making sure everything goes smoothly according to a solid, scientific plan, not just a hunch.
The Science Behind Effective Healing
Research has shed light on how our cells repair themselves. Take inflammation, for example. At first, it's vital for cleaning the wound. But if it sticks around too long, it can actually slow things down. Evidence-based wound care gives us ways to manage inflammation, keeping it helpful without letting it get out of control. For more on healing deep wounds, check out this helpful resource: How to Heal Deep Wounds Faster.
Moisture balance is another key player. Too much moisture can make the skin soggy, while too little dries out the wound bed. Research shows that a slightly moist environment is like the Goldilocks zone for cells – just right for optimal function and faster healing. Evidence-based wound care focuses on moisture management to create this ideal healing setting.
And let’s not forget about the tiny residents in our wounds: bacteria. Some bacteria are helpful for healing, but too many of the wrong kind can cause infection. Evidence-based wound care includes ways to prevent and control infection, keeping harmful microbes at bay.
From Reactive to Proactive Care
Evidence-based wound care represents a big shift from reacting to problems to preventing them in the first place. Traditionally, wound care often involved a lot of trial and error, dealing with issues as they popped up. But now, we can anticipate potential complications and step in early. This proactive approach reduces the risk of serious problems like infections and chronic wounds.
The results speak for themselves. One study showed that implementing evidence-based wound care dramatically reduced wound infection rates. Between 2017 and 2019, infections plummeted by 84.3%, from 7.3% to 1.3%. That’s a huge improvement in patient care. You can dive deeper into these findings here.
Real-World Impact of Evidence-Based Wound Care
Evidence-based wound care isn't just theory; it has real, tangible benefits for patients:
-
Faster Healing: By creating the optimal healing environment and addressing potential problems proactively, wounds heal more efficiently.
-
Reduced Pain and Discomfort: Effective wound management minimizes pain and improves patient comfort.
-
Improved Quality of Life: Faster healing and less pain mean patients can get back to their lives sooner.
-
Decreased Healthcare Costs: Preventing complications and promoting efficient healing reduces the need for expensive treatments and long-term care.
Ultimately, evidence-based wound care isn't just about healing wounds; it's about restoring well-being. It's about providing the best possible care, guided by science and tailored to each patient's individual needs. This focus on quality and patient-centered care is at the heart of modern wound healing.
Clinical Protocols That Actually Work In Practice
Think of clinical protocols in wound care like a well-worn cookbook. They provide the fundamental recipes for successful healing, offering guidance and structure while still allowing for flexibility based on the unique "ingredients" of each patient's situation. They aren't rigid rules, but adaptable frameworks grounded in the best evidence-based practices.
Inside Top-Performing Wound Care Facilities
Let's take a look inside some of the most successful wound care facilities. What sets them apart? They've embraced a systematic approach, implementing structured protocols for everything from initial assessments to treatment selection and ongoing progress monitoring. They've discovered that standardized care pathways take the guesswork out of wound care and dramatically improve patient outcomes.
For example, imagine two chefs preparing the same dish. With a standardized recipe, they'll achieve consistent results, regardless of their individual techniques. Similarly, a consistent wound assessment protocol ensures every caregiver evaluates a wound using the same criteria. This reduces the chance of overlooking critical details and leads to more accurate treatment decisions, even when different caregivers are involved over time. You might be interested in: Treating Diabetic Foot Ulcers.
Building Protocols That Deliver Results
Developing effective clinical protocols requires careful planning. Think of it like constructing a building – you need a solid foundation and a well-defined blueprint. Here are some key elements to consider:
- Clear Assessment Criteria: Just as a builder needs precise measurements, define specific parameters for evaluating wound characteristics. Think size, depth, tissue type – the vital stats of a wound. This allows for consistent data collection and informed decision-making.
- Evidence-Based Treatment Algorithms: These are your step-by-step instructions, drawn from the latest research, ensuring that treatment choices align with proven methods. Think of it as following a trusted recipe, knowing it’s been tested and refined for optimal results.
- Regular Progress Tracking: Like checking the progress of a construction project, implement a system for monitoring healing progress. Ideally, use objective measurements like wound area reduction. This enables early detection of potential problems and allows for adjustments to the care plan.
- Team Training and Education: Equipping your team with the knowledge and skills to implement the protocols is crucial. Ongoing training reinforces best practices and ensures consistent application, much like regular training ensures a construction crew works together effectively.
To help visualize how these elements fit together, let’s look at a practical example:
Key Clinical Protocol Components
| Protocol Element | Implementation Timeline | Success Metrics | Common Challenges |
|---|---|---|---|
| Standardized Wound Assessment | Within 24 hours of admission/initial visit | Consistent documentation of wound characteristics across all caregivers | Variations in individual assessment techniques |
| Evidence-Based Dressing Selection | At each dressing change | Decreased wound size, improved tissue quality | Keeping up-to-date with the latest research on dressing types |
| Pain Management Protocol | Implemented at initial assessment and reassessed regularly | Patient-reported pain scores, observation for nonverbal pain cues | Balancing pain relief with potential side effects of medications |
| Infection Prevention Strategies | Ongoing throughout treatment | Reduced incidence of wound infections | Ensuring adherence to hand hygiene protocols and aseptic technique |
This table highlights the key elements of a clinical protocol, the timeframe for their implementation, how success is measured, and the typical hurdles encountered. It's a snapshot of how structure and measurement drive effective wound care.
How Standardized Care Elevates Outcomes
Implementing standardized care pathways, built on these clinical protocols, brings numerous benefits:
- Reduced Variability: Consistency minimizes variations in care, much like using a standardized recipe yields predictable results in cooking.
- Improved Efficiency: Clear guidelines streamline the decision-making process, saving time and resources.
- Enhanced Communication: Standardized terminology and procedures improve communication between caregivers, minimizing confusion.
- Better Patient Outcomes: Ultimately, evidence-based protocols lead to faster healing, fewer complications, and happier patients. One study found that evidence-based nursing interventions significantly reduced the incidence of pressure injuries in ICU patients by a remarkable 78% compared to standard care.
Practical Tips for Protocol Implementation
Putting clinical protocols into daily practice requires a practical approach. Here's how:
- Start Small: Begin by implementing protocols for a specific wound type or patient group. Gradually expand as your team gains experience. Think of it like mastering one recipe before tackling a whole cookbook.
- Use Visual Aids: Flowcharts, checklists, and other visual tools can help caregivers quickly understand and apply the protocols.
- Regularly Review and Update: Medicine is always evolving. Ensure your protocols stay current with the latest research and best practices. Scheduled reviews help incorporate new knowledge and address any implementation challenges.
By following these steps, you can create clinical protocols that not only meet evidence-based standards but also work seamlessly within your setting. This translates research into action, making wound care a more predictable, efficient, and patient-centered process with tangible improvements.
Overcoming Real-World Implementation Challenges

Evidence-based wound care isn't a fixed recipe. It's more of a well-stocked toolkit. Just like a carpenter uses the same basic tools differently for building a birdhouse versus a bookshelf, healthcare providers adapt these principles to various situations and available resources. Let's explore how they’re making it work across the globe.
Adapting to Resource Limitations
Access to advanced wound care supplies can be a real hurdle in many areas. But that doesn't make evidence-based care impossible. Imagine a rural clinic with limited resources. Something as simple as saline dressings, changed regularly following best practices, can surprisingly outperform infrequent changes of expensive, high-tech dressings.
This underscores a key idea: consistent basic care, done right, can be more effective than inconsistent complex interventions.
In these settings, providing good wound care can be especially tough, but it remains essential for improving patient outcomes. A study in India found chronic wounds in 4.48 per 1,000 people and acute wounds in 10.55 per 1,000 people, highlighting the urgent need for effective solutions. Learn more from this resource.
Blending Traditional and Modern Practices
Traditional healing methods hold deep significance in many cultures. Instead of discarding these practices, evidence-based wound care looks for ways to integrate them. Think of certain herbal remedies proven to have antibacterial or anti-inflammatory properties. By combining these with modern dressings and techniques, providers can create treatment plans that are both effective and culturally sensitive.
Ingenuity in Action: Real-World Examples
Healthcare professionals worldwide are constantly finding inventive ways to apply evidence-based wound care. In one urban hospital facing budget cuts, nurses created a peer-to-peer training program on proper wound assessment. This boosted consistency in care across different shifts and actually reduced hospital-acquired pressure injuries.
In another case, a rural clinic team devised a simple system for remote monitoring. Patients sent photos of their wounds via mobile phone, enabling early intervention and fewer costly hospital visits. For more on how home care can benefit recovery, see our guide on How Home Wound Care Speeds Up Recovery.
Empowerment Through Flexibility
These stories show that evidence-based wound care is not a rigid set of rules, but a flexible framework. It empowers providers to find innovative solutions that truly fit their unique circumstances. This adaptability is vital to ensure everyone, regardless of location or resources, benefits from the best possible care. By embracing these principles, we can create patient-centered solutions that improve healing and enhance quality of life.
Advanced Tools That Change The Game

This screenshot from WoundSource illustrates the many different types of chronic wounds. It's a good reminder of just how prevalent and complex these conditions can be, often requiring specialized and advanced care. The site provides valuable resources for both patients and healthcare professionals.
The image underscores the importance of understanding that not all wounds are created equal. Each type of chronic wound – from pressure injuries to diabetic ulcers – demands a unique approach within the broader framework of evidence-based wound care. This naturally leads us to the need for advanced tools and the specialized knowledge to use them effectively. So, let's explore some of these exciting advancements.
Bioengineered Skin Substitutes: A Second Skin
Imagine trying to repair a tear in your favorite shirt. A simple patch might work sometimes, but if the damage is extensive, you might need a whole new section of fabric. Bioengineered skin substitutes offer a similar solution for wounds. These aren't your everyday bandages. They're actually living tissues, carefully engineered to mimic the properties and functions of real skin. Think of them as providing a scaffold that encourages new cells to grow, accelerating the healing process, especially for tricky wounds like severe burns or stubborn diabetic ulcers.
This technology represents a significant leap forward in evidence-based wound care. It provides a more effective way to repair damaged tissue, offering hope for patients who previously faced long and difficult healing journeys.
Negative Pressure Wound Therapy: Vacuum-Assisted Healing
Picture a vacuum cleaner pulling dirt and debris from a carpet. Negative pressure wound therapy (NPWT), often called vacuum-assisted closure, operates on a similar principle, albeit much more gently, to promote wound healing. A specialized dressing is placed over the wound and connected to a vacuum pump. This creates gentle suction that removes excess fluid and stimulates blood flow to the wound bed.
The result? A cleaner, healthier environment that’s conducive to healing. The gentle suction also helps draw the wound edges closer together. NPWT is a powerful example of how evidence-based wound care integrates technology to accelerate the healing process and minimize the risk of infection.
Smart Wound Dressings: The Future of Wound Monitoring
What if a bandage could alert you to a wound infection even before you see any visible signs? That's the promise of smart wound dressings. These dressings are embedded with tiny sensors that constantly monitor key factors like temperature, pH levels, and even the presence of bacteria.
This real-time data provides healthcare professionals with invaluable insights into the wound's condition, allowing them to adjust treatment strategies proactively. This early detection capability is crucial in evidence-based wound care, enabling timely interventions that can prevent complications before they escalate.
Choosing the Right Tool for the Job
It's important to remember that these advanced interventions aren't a one-size-fits-all solution. The decision to use a particular tool depends on several factors, including the type of wound, the patient's overall health, and the resources available. Just like a carpenter selects specific tools for different tasks, healthcare professionals carefully evaluate each patient's unique needs when choosing advanced wound treatments.
This individualized approach ensures that the chosen intervention aligns with evidence-based principles and the patient's particular circumstances. Cost is another critical consideration. These advanced tools can be expensive, so open and honest discussions about the potential benefits and financial implications are essential for responsible, patient-centered care.
Bringing Evidence-Based Care Beyond Hospital Walls
Extending evidence-based wound care into homes and long-term care facilities presents unique challenges. It requires adapting hospital-level standards to less structured environments. Think of it like trying to bake a soufflé in a moving car – it demands resourcefulness, adaptability, and a dash of ingenuity. But with the right approach, success is entirely achievable.
Bridging the Gap Between Clinic and Home
One of the biggest hurdles is replicating the controlled environment of a hospital. Maintaining consistent wound care in a bustling home, with its unpredictable interruptions and distractions, can be tough. It’s like trying to conduct a symphony orchestra in a noisy playground – focus and precision become paramount.
This is where telemedicine shines. It allows specialists to connect with patients remotely, offering expert guidance and monitoring progress without the need for constant in-person visits. It’s like having a virtual coach guiding the patient and their caregivers through the healing process. Furthermore, family caregiver training programs become invaluable, empowering family members with the skills and knowledge to provide consistent, quality care at home.
Empowering Family Caregivers
Equipping non-clinical caregivers is essential. Think of it like teaching someone to sail. They need to understand not just how to adjust the sails, but why – how wind direction and water currents impact the boat’s movement. Similarly, caregivers need to grasp the reasons behind each step in the wound care process. Explaining the importance of hand hygiene helps them understand its impact on infection risk, while demonstrating proper dressing techniques prevents further injury. For more insights on home health wound care outcomes, check out Windy City Wound Care.
Remote Monitoring Systems: Keeping a Virtual Eye on Healing
Remote monitoring systems provide an extra layer of support. These systems use sensors and wearable technology to track vital signs and wound status, sending real-time data to healthcare providers. Imagine a gardener with sensors in their garden, alerting them to changes in moisture levels – they can address potential issues before they escalate. Similarly, these systems allow for timely interventions, preventing minor problems from blossoming into major setbacks. This proactive approach is a cornerstone of evidence-based care, reducing the need for costly emergency room visits and hospital readmissions.
Success Stories: Evidence in Action
Real-world examples illustrate the effectiveness of these strategies. One home healthcare agency combined telemedicine visits with caregiver training and saw a dramatic decrease in wound-related hospitalizations and a significant increase in patient satisfaction. The program not only improved healing but also empowered patients and families to actively participate in their care.
Another program focused on delivering pre-packaged wound care kits directly to patients’ homes. This simplified dressing changes and ensured access to the necessary supplies. Think of it like having a pre-portioned meal kit – everything is measured and ready to go, minimizing errors and streamlining the process. The result? Improved adherence to treatment plans and fewer complications.
Ensuring Continuity of Care
Transitioning between care settings, like moving from a hospital to a long-term care facility or home, demands careful coordination. This is crucial for maintaining evidence-based practices. Clear communication between healthcare providers across different settings is essential. It's like a relay race – a smooth handoff of the baton is critical for a winning outcome.
Practical Strategies for Managing Supplies and Resources
Efficient supply management is another key component. Imagine an artist running out of paint mid-stroke – it disrupts the creative flow. Similarly, in wound care, having the right supplies at the right time is crucial. Here are a few practical strategies:
- Centralized Supply Management: Create a system for ordering, storing, and distributing supplies, ensuring easy access and preventing shortages.
- Pre-packaged Wound Care Kits: These streamline dressing changes and minimize waste.
- Inventory Tracking: Regularly monitor supply levels to anticipate needs and avoid delays.
By embracing these strategies and learning from real-world successes, we can extend the reach of evidence-based wound care, bringing its benefits to those who need it most. This commitment to quality care, regardless of setting, empowers patients and improves lives.
Tracking Success and Getting Better Every Day
Imagine you're tending a garden. You wouldn't judge its success solely on the final flowers, would you? You'd watch the entire process unfold – from tiny sprouts to vibrant blooms. Similarly, evaluating wound care requires a comprehensive approach. It’s not just about closure. It's about improved quality of life, reduced pain, and increased patient satisfaction.
Building Measurement Systems That Drive Improvement
Effective healthcare organizations are like master gardeners. They don’t just observe; they analyze. They track sunlight, soil composition, and watering frequency to optimize growth. In wound care, this translates to monitoring healing rates, infection occurrences, and patient-reported pain levels. These insights are crucial for improving care.
These measurements should capture both the objective and the subjective. Think wound size reduction in centimeters paired with a patient's comfort level on a pain scale. This two-pronged approach gives a complete picture of the healing journey.
Using Data to Uncover Opportunities for Better Care
Data analysis is a powerful tool, acting like a magnifying glass to reveal hidden opportunities. Let's say a hospital notices a rise in surgical site infections. By analyzing data on operating room procedures, sterilization techniques, and post-op care, they might uncover a flaw in their infection control process.
This data-driven approach allows for targeted improvements. For example, if data reveals delays in dressing changes at a long-term care facility, implementing a more efficient workflow could dramatically improve healing outcomes.
Practical Approaches to Data Collection and Interpretation
Collecting useful data doesn’t require complex systems. Simple tools like wound measurement charts, pain scales, and patient satisfaction surveys offer valuable insights. The key is consistency. Think of a chef meticulously documenting ingredients and cooking times to perfect a recipe. The same principle applies to wound care data collection.
Interpreting this data also requires careful consideration. A slow healing rate might signal an underlying infection, requiring a shift in treatment strategy. It's like a detective piecing together clues to solve a case.
Refining Protocols and Training Programs for Sustained Excellence
Evidence-based wound care is a continuous journey of improvement. Data analysis informs updates to protocols and training programs. Picture a sports team reviewing game footage to pinpoint weaknesses and improve their strategy. Similarly, healthcare organizations use wound care data to identify areas where their protocols or training could be enhanced.
This commitment to ongoing learning sets evidence-based wound care apart. It's about constantly striving for better ways to heal, using data as a compass to achieve the best possible outcomes for every patient. This translates to better patient experiences, faster healing, and a higher overall quality of care.
Looking for expert wound care tailored to your needs? Rapid Wound Care offers comprehensive at-home services designed for your comfort and recovery. Connect with us today to learn more: Rapid Wound Care

