Pressure ulcers, which many know as bedsores, are a serious and painful—but almost always preventable—medical problem. Imagine a constant, unyielding weight on one spot of your skin. It acts like a roadblock on a tiny, vital highway, cutting off blood flow and starving the tissue of the oxygen and nutrients it needs to survive. Eventually, that tissue just breaks down.
Following proven pressure ulcer prevention guidelines isn’t just about checking a box; it’s a cornerstone of patient safety and compassionate care.
Why Pressure Ulcer Prevention Is Not Negotiable
Think of this guide as your roadmap to preventing those roadblocks. We’re going to skip the dry, academic definitions and get straight to the actionable, evidence-based strategies that healthcare teams and family caregivers can use today. The mission is to build a proactive culture where preventing these wounds becomes second nature.
When we fail to prevent a pressure ulcer, it’s not just a clinical setback. It’s a profound blow to a person’s dignity and well-being. Compromised skin opens the door to severe pain, dangerous infections, and a sharp decline in quality of life. What might have been a manageable health issue can quickly spiral into a complex, long-term battle for recovery.
The Foundation of Modern Prevention
Effective prevention isn’t guesswork. It's built on a solid foundation of globally recognized standards that have been tested and proven in the real world. For example, the International Guidelines for pressure ulcer prevention and treatment have been a guiding force in clinical practice since 2009. These standards, cited over 2,800 times in scientific literature, are constantly updated to keep pace with new research. To see how these protocols continue to evolve, you can explore the work on the upcoming fourth edition.
The data tells a powerful story.
A major meta-analysis compared outcomes between two groups: one receiving standard care and another using evidence-based nursing interventions. The results were staggering. In the evidence-based group, only 4% of patients developed a pressure ulcer. In the conventional care group, that number jumped to 18%.
This isn't a small difference. It shows just how effective a structured, proactive approach can be.
Key Pillars of Proactive Care
A successful prevention strategy is a team effort. It’s not about one single action, but a bundle of consistent, coordinated interventions that work together. Success really boils down to getting these core components right:
- Systematic Risk Assessment: The first line of defense is identifying who is at risk from the very beginning.
- Diligent Skin Care: Daily skin inspections and proper hygiene are crucial for maintaining the skin's natural, protective barrier.
- Consistent Repositioning: For anyone with limited mobility, regularly relieving pressure is absolutely non-negotiable.
- Proper Nutrition and Hydration: You can't build strong, resilient skin from the outside alone. It starts from within.
By mastering and applying these principles, caregivers create an environment where pressure ulcers simply struggle to form. This guide will walk you through each of these critical areas, giving you the practical steps needed to turn these guidelines into life-saving action.
For an even deeper dive into wound care topics, feel free to explore our comprehensive wound care knowledge base.
Mastering Risk Assessment to Predict and Prevent
Strong pressure ulcer prevention always starts with one critical step: figuring out who is most vulnerable in the first place. You can think of this less like a simple checklist and more like a form of predictive analysis. The goal is to spot the warning signs long before any skin damage appears, allowing us to jump in with proactive, targeted support.
This isn't about slapping a generic plan on everyone. It’s a dynamic process that means understanding each person's unique mix of risk factors. Two patients could be at risk for completely different reasons, and those reasons demand entirely different strategies.
Decoding Risk with the Braden Scale
To bring some structure to this process, healthcare professionals lean on a tool called the Braden Scale. This isn't just another form to fill out; it's a systematic way to evaluate six key areas that directly influence the risk of skin breakdown. When you understand these components, you can turn abstract risks into a concrete, personalized prevention plan.
The image below shows how a clinician uses a tool like the Braden Scale to build a patient-specific risk profile.
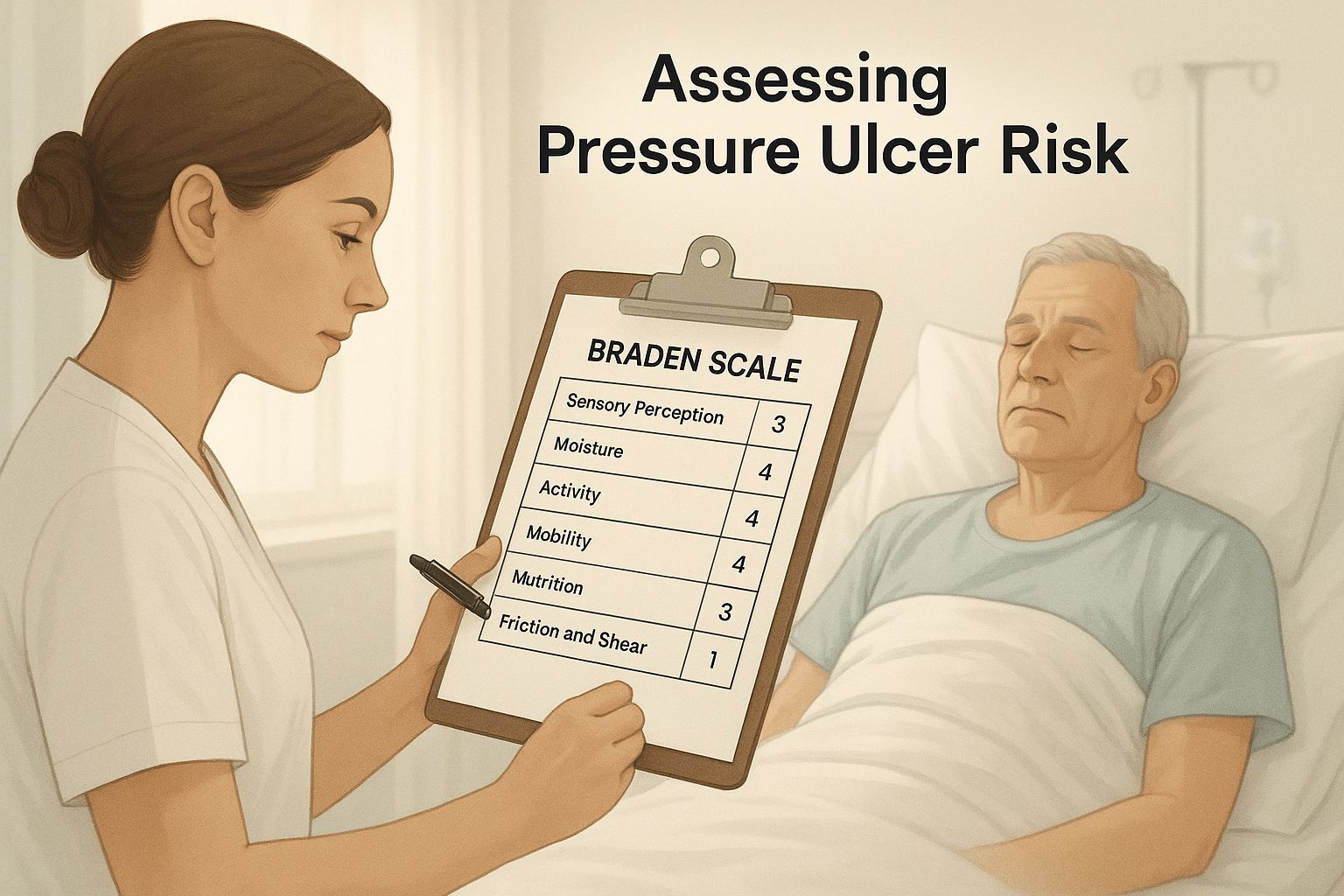
As you can see, assessment is an active, hands-on process. It’s about combining sharp clinical observation with structured evaluation to keep the patient safe.
The Six Pillars of Risk Assessment
Let's break down the six factors the Braden Scale helps us evaluate. Each one is a piece of the puzzle, and a low score in any single area signals a potential weakness in the body’s natural defenses against pressure.
- Sensory Perception: This is all about a person's ability to feel and react to pain or pressure-related discomfort. Someone who can't sense that they need to shift their weight is at a much higher risk.
- Moisture: Skin that's constantly damp from sweat, urine, or wound drainage becomes soft, fragile, and far more likely to break down.
- Activity: This looks at a person’s overall degree of physical activity. If someone is bed-bound or confined to a chair, they have very few opportunities to relieve pressure on their own.
- Mobility: This is different from activity. Mobility focuses on the ability to change and control body position. A person might be active but have limited mobility in certain areas due to paralysis or severe pain.
- Nutrition: The body needs good fuel—protein, calories, and vitamins—to keep skin healthy and repair minor damage before it gets worse. Poor nutrition is like trying to build a strong brick wall with weak, crumbling mortar.
- Friction and Shear: These two are troublemakers. Friction is the rubbing of skin against a surface, like when someone is pulled up in bed. Shear happens when the skin stays put but the underlying bone moves, which stretches and tears the tissues and blood vessels underneath.
A lower total score on the Braden Scale means a higher risk. For adults, a score of 18 or below is a clear signal that preventive measures need to start immediately.
To put these factors into perspective, here’s a quick look at who is most vulnerable.
Key Risk Factors for Pressure Ulcer Development
| Risk Factor Category | Description | High-Risk Patient Example |
|---|---|---|
| Immobility & Inactivity | Unable to change position independently, confining pressure to bony areas. | A patient in a coma or with quadriplegia who is fully dependent on caregivers for repositioning. |
| Poor Sensory Perception | Cannot feel discomfort or pain, so the natural trigger to move is absent. | An individual with advanced diabetic neuropathy who has lost sensation in their feet and lower legs. |
| Malnutrition & Dehydration | Lack of protein, calories, and fluids weakens the skin and impairs its ability to heal. | An elderly patient with a poor appetite who is not consuming enough protein or staying hydrated. |
| Excessive Moisture | Constant exposure to sweat, urine, or feces macerates the skin, making it fragile. | An incontinent patient whose skin is frequently exposed to moisture without a proper barrier cream. |
| Friction & Shear Forces | Mechanical forces that stretch or rub the skin, damaging underlying tissue and blood vessels. | A patient who frequently slides down in bed, creating shear forces on their sacrum and heels. |
Understanding these categories helps clinicians move from a general score to a specific, actionable plan tailored to the individual's biggest threats.
Clinical studies have shown just how powerful this is. A major analysis found that implementing structured prevention protocols, starting with a solid risk assessment, caused the rate of new ulcers to plummet from 18% in conventional care settings to just 4%.
This is huge. It proves that risk assessment isn't just paperwork—it's the first and most effective action in any successful prevention strategy.
Risk Assessment Is a Continuous Conversation
Here’s something that can’t be stressed enough: a person's risk level isn't set in stone. It can change, and sometimes, it can change fast.
An individual who was low-risk when they arrived might become high-risk after a surgery, a change in medication, or a dip in their nutritional intake. Because of this, risk assessment has to be a continuous process, not a one-and-done task at admission.
Reassessment should happen:
- On admission to get a baseline.
- On a regular schedule, like weekly in long-term care or even daily in the ICU.
- Whenever there is a significant change in the patient’s condition.
When we treat risk assessment like an ongoing conversation, we can adapt our prevention strategies in real time. This ensures the care plan always matches the patient's current level of vulnerability—and that's the key to stopping pressure ulcers before they ever get a chance to form.
Your Guide to Proactive Skin Integrity Management
Think of a patient's skin as the body's first and most important line of defense. Like any vital organ, it needs consistent, careful attention to stay strong and protect the body from harm. This is where proactive skin integrity management comes in—it’s a core piece of any serious pressure ulcer prevention guidelines and your best strategy for stopping damage before it starts.
This isn't about reacting to problems after they appear. It's about creating an environment where the skin can truly thrive. The entire approach is built on a foundation of simple but powerful daily habits, from gentle cleansing to smart moisture control. Mastering these skills is absolutely essential for keeping the skin’s natural barrier tough and resilient.

The Daily Head-to-Toe Skin Inspection
You can't protect what you don't see. The first step in maintaining healthy skin is knowing its current state, which makes a daily, systematic head-to-toe inspection non-negotiable, especially for at-risk individuals. This routine check helps you catch the subtle signs of trouble long before a pressure ulcer has a chance to form.
When you're inspecting the skin, you need to look for more than just obvious redness. Pay close attention to these early warning signs:
- Temperature Changes: An area that feels warmer or cooler than the skin around it could signal inflammation or poor blood flow.
- Texture and Firmness: Skin that feels spongy, boggy, or unusually firm can be a red flag for damage happening in the deeper tissue layers.
- Color Variations: On lighter skin, this often looks like redness that doesn't fade. On darker skin tones, where redness is harder to spot, look for purple, bluish, or shiny patches.
This daily habit acts as your early warning system. It turns a quick glance into an active search for the first signs of distress, giving you the chance to intervene immediately.
Gentle Cleansing The Right Way
The goal here is simple: remove irritants without stripping the skin of its natural, protective oils. Unfortunately, many common, alkaline soaps do more harm than good. They disrupt the skin's delicate pH balance, leaving it dry, brittle, and wide open to injury.
The solution is to switch to gentle, pH-balanced cleansers. Always use lukewarm water—never hot—and avoid aggressive scrubbing that creates friction and can tear fragile skin. Afterward, gently pat the skin dry with a soft cloth, making sure to get into skin folds where moisture loves to hide.
A healthy skin barrier is the body's first line of defense. When this barrier is compromised by harsh cleansing agents or excessive moisture, its ability to resist damage from pressure and shear diminishes significantly.
This small change from a harsh soap to a gentle cleanser is a fundamental step in preserving the skin's natural strength. It's a minor adjustment that delivers major protection. For patients facing more complex skin issues, seeking professional help is crucial. You can learn more about expert wound care in Chicago to see how specialists handle these advanced conditions.
The Critical Role of Moisturizers
Dry skin is weak skin. It simply doesn't have the pliability and elasticity it needs to withstand the mechanical forces of pressure and shear. This is why moisturizers are such an indispensable tool in your prevention arsenal.
Applying an emollient right after bathing helps lock in hydration, keeping the skin soft, supple, and resilient. This improves its ability to stretch and move without tearing. To minimize the risk of irritation, always look for fragrance-free, hypoallergenic products. Think of it like conditioning a leather glove to keep it from cracking—moisturizer provides the same benefit for skin.
Managing Incontinence-Related Moisture
One of the biggest threats to skin integrity is prolonged exposure to moisture, especially from incontinence. This leads to a condition called incontinence-associated dermatitis (IAD), which makes the skin dramatically more vulnerable to breakdown from pressure.
An effective management plan is a three-part strategy:
- Cleanse Promptly: As soon as soiling occurs, gently clean the skin with a pH-balanced perineal cleanser.
- Apply a Barrier: Use a moisture barrier cream or ointment. These products create a protective seal that shields the skin from direct contact with urine and feces.
- Use Absorbent Products: Choose high-quality, absorbent pads or briefs that are designed to wick moisture away from the skin, keeping the surface as dry as possible.
Managing moisture consistently is a true cornerstone of preventing skin breakdown. By keeping the skin clean, properly moisturized, and protected from irritants, you create the best possible conditions for it to stay healthy and intact, even in challenging situations.
Using Support Surfaces and Repositioning to Beat Pressure
While diligent skin care lays the essential groundwork, the most powerful strategy in our playbook is to directly fight the primary enemy: uninterrupted pressure. This battle is won on two fronts: specialized support surfaces and consistent repositioning. When you use them together, they create a formidable defense that protects vulnerable tissue from the inside out.
Think about the classic "bed of nails" trick. How can someone lie on thousands of sharp points without a scratch? It's all about weight distribution. Spread out over a huge area, the pressure at any single point is tiny. But just one nail? That would be a different story.
This is the exact principle behind specialized support surfaces. They work by redistributing body weight to stop intense pressure from building up on bony hot spots like the heels, hips, and sacrum.

Choosing the Right Tools for the Job
Not all support surfaces are the same, and picking the right one comes down to the patient's specific risk level. Using the wrong surface is like bringing a garden hose to a five-alarm fire—it’s just not going to cut it.
- Static Surfaces: For patients at a low to moderate risk, a high-specification reactive foam mattress is often the go-to choice. We're not talking about those old-school egg crate toppers, which are no longer recommended. These modern mattresses are engineered with multiple layers of high-density foam that contour to the body, dramatically increasing the contact area and dialing down the pressure on those bony prominences.
- Dynamic Surfaces: When you're dealing with someone at high or very high risk, a dynamic support surface becomes non-negotiable. These are active systems, like alternating pressure mattresses, that use air cells to systematically inflate and deflate. This process is constantly shifting the points of pressure, making sure no single area has to bear the body's weight for too long.
The key here is matching the technology to the need. A static foam mattress is great for prevention in moderate-risk cases, but it can't hold a candle to the active pressure relief a dynamic mattress provides for someone who is completely immobile.
Repositioning: The Cornerstone of Prevention
Even with the most advanced mattress in the world, nothing beats movement. Regular repositioning is the single most critical intervention for anyone with limited mobility. The old "turn every two hours" rule is a decent starting point, but today’s best practices call for a more thoughtful approach.
The goal isn't just to turn, but to turn correctly. If you do it wrong, you can actually create new problems, especially from something called shear force.
What is Shear?
Imagine a patient sliding down in bed. Their skin sticks to the sheet, but their skeleton and deeper tissues keep moving downward with gravity. This internal stretching pulls and tears tiny blood vessels and soft tissue, causing devastating damage that you can't even see on the surface—until it’s far too late.
To fight both pressure and shear, the 30-degree lateral tilt position is the gold standard. Instead of rolling a patient a full 90 degrees onto their side (which just puts all the pressure on their hip bone), a 30-degree tilt supported by pillows or wedges gets them off their back without simply loading up a new bony spot.
Of course, some wounds require specific treatments, and it's important to know things like how to perform wet-to-dry dressing changes correctly, but preventing the injury from ever happening is always goal number one.
Building a Repositioning Schedule That Works
An effective turning schedule is more than just a time on a clock; it has to be a personalized plan. For someone in bed, every two hours is standard. But for those sitting in a chair—where pressure is far more concentrated—they should be shifting their weight every 15 minutes and be fully repositioned at least once every hour.
The good news? All this focused effort is actually making a difference. The global prevalence of pressure ulcers has seen a slight but encouraging decline. A 2025 study found the age-standardized prevalence rate dropped from 8.25 to 7.92 per 100,000 people between 1990 and 2021, with most cases affecting those over 60. This trend shows that when we apply these evidence-based guidelines, we see real, measurable improvements in patient safety.
By combining the right support surface with a smart, consistent repositioning schedule, you actively offload pressure, promote blood flow, and give the skin its best possible chance to stay healthy and intact.
How Nutrition and Hydration Build Resilient Skin
While turning schedules and specialized mattresses fight pressure from the outside, a truly complete prevention plan has to build strength from the inside out. Real skin resilience is an inside job, fueled by good nutrition and proper hydration. Without these core building blocks, the skin just doesn't have what it needs to stand up to pressure or repair itself.
Think of it like building a fortress. You can have the best design in the world, but if you build it with shoddy, brittle bricks and weak mortar, it’s going to crumble at the first sign of trouble. The body is no different—it can't create strong, healthy tissue without the right raw materials. This makes nutrition a non-negotiable part of any serious pressure ulcer prevention guidelines.
The Essential Building Blocks for Strong Skin
A well-fed body has a much, much better shot at fending off skin breakdown. Malnutrition literally starves the skin of the components it needs to stay intact and functional. A few key nutrients play starring roles here.
Zeroing in on these specific elements can make a world of difference:
- Protein: This is the absolute foundation of skin tissue. It provides the "bricks" needed to build and repair. If protein is low, the body can't replace old cells or fix minor damage, leaving skin fragile and weak.
- Calories: Energy runs everything, including cell turnover and healing. If calorie intake is too low, the body gets desperate and starts breaking down protein for fuel—stealing the very material the skin needs to stay strong.
- Vitamin C: This is the "mortar" that holds the skin's fortress together. It's absolutely critical for making collagen, the protein that gives skin its toughness and elasticity.
- Zinc: This mineral is a key player in making proteins and new cells. That makes it essential for both maintaining healthy skin and repairing any damage that pops up.
Putting Nutritional Support into Practice
Spotting a nutritional gap is just the first step; fixing it is where the real work begins. For at-risk individuals, especially those with a poor appetite or other health issues, this usually takes a team effort.
A multidisciplinary approach that includes a dietitian is crucial. They can run detailed nutritional assessments and create personalized plans to fix specific shortfalls, making sure the patient gets exactly what their body needs to build resilience from within.
Here are a few practical ways to make sure intake is solid:
- Offer Nutrient-Dense Foods: Focus on meals and snacks packed with protein, vitamins, and minerals. Think lean meats, fish, eggs, dairy, beans, and leafy greens.
- Use Oral Nutritional Supplements: When someone can't get enough from their diet alone, high-protein, high-calorie shakes or puddings are a simple and effective way to bridge the gap.
- Track Fluid Intake: Dehydration is a huge enemy of healthy skin. It reduces skin plumpness (turgor) and hurts circulation, making tissue way more vulnerable to injury. Aim for steady hydration all day long, keeping a close eye on intake and output.
Connecting Nutrition to Overall Care
A solid nutritional plan doesn't just help the skin—it makes every other prevention strategy you're using even more effective. It gives the body the strength to handle being repositioned and provides the fuel to heal tiny injuries before they blow up into big problems.
If you're overseeing care at home, getting a handle on these principles is a game-changer. For a deeper dive, checking out resources on pressure ulcer treatment in a home care setting can offer some incredibly valuable and specific advice. At the end of the day, making nutrition and hydration a core part of your daily care plan is one of the most powerful moves you can make to protect vulnerable skin.
Putting Guidelines Into Practice for Lasting Success
Knowing the official pressure ulcer prevention guidelines is one thing. Actually weaving them into the day-to-day chaos of a busy clinical setting? That's the real challenge.
Success isn't about one superstar nurse or a single checklist. It’s about building a genuine culture of safety where everyone—from nursing aides and physicians to the patient's own family—feels empowered and responsible. This shift from simply knowing the rules to actively doing the work is what creates lasting change.
Think of it like a symphony orchestra. For the music to sound right, every musician has to play their part perfectly, on cue, and in harmony with everyone else. In the same way, every single repositioning, skin check, and nutritional tweak has to be done reliably by every person on the team.
Creating a System of Accountability
To make that kind of consistency happen, you need rock-solid documentation. This isn't just about CYA or checking a box for compliance. It's about clear communication. Detailed, real-time notes on repositioning schedules, skin assessments, and any interventions create a living record of care. This allows the entire team to track progress and, more importantly, spot trouble before it spirals.
This data-driven mindset lets you see what’s working and what isn't. By tracking your facility's pressure ulcer incidence rates and comparing them against your prevention efforts, you create a powerful feedback loop that drives constant improvement.
Even with the best game plan, pressure ulcers can still happen. When they do, the goal isn't to point fingers. It's to learn. A thorough root cause analysis helps the team dig into the "why" behind the event, uncovering any weak spots in the system that need fixing.
This commitment to improvement is a shared responsibility. When a pressure ulcer does develop, it's an opportunity for collective learning, prompting a review of processes to strengthen defenses for all patients moving forward.
Overcoming Systemic Hurdles
Of course, putting these strategies into action requires buy-in from the entire organization, and sometimes outside policies can throw a wrench in the works. For instance, in the United States, various measures have tried to nudge hospitals toward better prevention using financial incentives and penalties, but the results have been a mixed bag.
In one key federal program, pressure ulcers were given a relatively low weight—just 6%—in a composite score for hospital-acquired conditions. This may have unintentionally pushed them down the priority list compared to other issues. You can read more about how policy impacts prevention rates to see how these big-picture factors influence what happens at the bedside.
Ultimately, a strong prevention culture is built from the inside out, grounded in a shared belief that patient safety is non-negotiable. When a wound does occur despite your best efforts, knowing what to do next is critical. For more on responsive care, you might find our guide on how to heal deep wounds faster helpful.
By empowering every team member to be a champion for prevention, you can build a system that protects every patient with the safe, proactive care they deserve.
Here is the rewritten section, crafted to match the human-written, expert tone and style of the provided examples.
Common Questions About Pressure Ulcer Prevention
Even with the best guidelines, real-world situations bring up questions. Having clear, straightforward answers is key to building confidence—both for clinical teams and for family members trying to provide the best care at home.
Let’s tackle some of the most common questions we hear on the ground.
How Often Should a High-Risk Patient Be Repositioned?
The classic rule of thumb for a high-risk person in bed is to reposition them at least every two hours. This simple act is incredibly powerful—it gives compressed skin a chance to breathe and restores vital blood flow.
But think of that two-hour schedule as a starting point, not a rigid rule. The right timing really depends on the person. We have to consider their skin's tolerance, the type of mattress they're on, and their overall health. For someone sitting in a chair, where pressure is far more concentrated, the need is even greater—they should be shifted at least every hour.
If there's one thing we've learned from decades of wound care, it's that consistency is everything. Even the most advanced mattress can’t do its job if a patient is left in one position for too long. Regular movement is non-negotiable.
Are Egg Crate Foam Mattresses Good for Prevention?
They used to be everywhere, but the simple answer is no. Standard egg crate foam overlays are no longer recommended by international guidelines for preventing pressure ulcers. While they might add a bit of comfort, they just don’t have what it takes to effectively redistribute pressure.
Modern prevention relies on technology designed specifically for the job:
- High-specification foam mattresses are the standard for people at a moderate risk.
- Dynamic support surfaces, like alternating pressure mattresses that actively shift air, are essential for those at high risk.
These surfaces are engineered to spread body weight out, drastically reducing the intense pressure on bony areas like the heels and tailbone.
What Is the First Sign of a Pressure Ulcer?
The earliest warning sign is usually non-blanching erythema. It sounds technical, but it’s simple to spot: a patch of red skin that stays red even when you press on it. A normal flush would turn white for a moment and then return to red; this doesn’t.
That patch of skin might also feel different—warmer, cooler, or firmer than the surrounding area. These subtle changes in texture and temperature are especially important clues for individuals with darker skin tones, where simple redness can be very difficult to see. Catching an injury at this stage is the absolute key to stopping a serious wound before it starts.
At Rapid Wound Care, we believe in proactive, expert care delivered right to your door. If you are managing complex wounds or need specialized support to prevent pressure injuries, our team is ready to help. We bridge the gap between patients, primary care, and wound specialists, ensuring you get the right treatment at the right time.
Find out how we can support your healing journey at https://rapidwoundcare.com.

