Understanding Your Body's Healing Roadblocks
Imagine your body is trying to complete a major construction project: healing a wound. Your cells are the dedicated crew, ready with all the right materials. But the job site is a mess. It’s cluttered with old, dead materials, occupied by bacterial squatters, and blocked by debris. With all these roadblocks, no new foundation can be laid. This is exactly what happens when a wound gets stuck and stops healing.
Why Some Wounds Get 'Stuck'
When a wound doesn’t follow the normal stages of healing, it can become a chronic problem. This isn't a sign that your body has given up. Instead, it’s fighting a losing battle against very real physical barriers that stand in the way. The two main culprits are:
- Necrotic Tissue: This is dead tissue that has no blood supply. It serves as an open invitation for bacteria and physically blocks healthy new cells from moving in and rebuilding the area.
- Biofilm: Think of this as a slimy, highly organized colony of bacteria. It sticks firmly to the wound's surface and is incredibly resistant to both your immune system and antibiotics.
A wound debridement procedure is like calling in a professional cleanup crew. A specialist arrives on-site to methodically clear away all the debris, giving the healing process a fresh start. This intervention clears the path so that reconstruction can finally begin.
The image below shows a dramatic before-and-after example of what debridement accomplishes.
Notice how the dark, non-viable tissue (eschar) has been completely removed. This exposes the healthier, pink tissue underneath, creating a clean wound bed that is finally prepared for the next stages of healing.
A Time-Tested Medical Necessity
Clearing away these healing roadblocks isn't some new medical trend; it’s a foundational practice that has saved lives for centuries. The wound debridement procedure evolved from battlefield medicine into a cornerstone of modern wound care. In the late 19th century, a Russian military surgeon named Carl von Reyher was the first to formally define this technique of mechanically cleaning wounds.
During the Russo-Turkish wars, his consistent use of debridement led to a remarkable 43% reduction in mortality among injured soldiers. This proved just how critical the procedure was. You can find more details in this excellent overview of debridement's history.
Debunking Common Debridement Myths
Even with its proven success, some common myths about debridement persist. One is the old belief that all wounds heal best if left alone to "air out." For a complex wound, this approach actually allows harmful barriers to build up and stall recovery.
Another myth is that debridement is just a form of aggressive cleaning. In reality, it is a precise medical intervention performed by a trained professional. The goal is to selectively remove only the non-viable tissue while carefully preserving the healthy structures underneath. This targeted removal is what makes it a medical procedure, not just simple wound washing.
Understanding this difference is vital. Debridement actively takes down the barriers that are stopping your body from doing its job. It essentially resets the healing clock, allowing your natural repair systems to take over. For chronic wounds that have been stuck for weeks or months, it is often the single most important step toward recovery. To learn what comes next, you can check out our guide on how to heal deep wounds faster and support the entire recovery process.
Five Debridement Methods That Actually Work
A healthcare provider chooses a specific wound debridement procedure much like a master carpenter selects the right tool for a delicate job—it must be perfect for the task at hand. No single method fits every wound. The best approach is always matched to your wound's specific condition, your overall health, and the ultimate treatment goals. This careful selection is a blend of medical science and hands-on experience, designed to ensure the best possible healing outcome.
Sharp Debridement: The Precision Approach
Think of this as a surgical mission with a very clear target. Sharp debridement involves using sterile instruments, such as scalpels or scissors, to quickly and precisely remove dead or non-viable tissue. As the fastest method available, it is often the first choice for large wounds or when an infection is a serious concern. This technique demands a high level of skill to make sure healthy tissue is preserved. Its roots are deeply tied to major surgical advancements, where refined instruments paved the way for more effective wound management. Discover more about these historical innovations here.
Enzymatic Debridement: The Targeted Dissolver
If sharp debridement is surgery, then enzymatic debridement is like applying a highly specific cleaning gel. In this method, a prescription ointment containing special enzymes is applied directly to the wound. These enzymes go to work, breaking down and liquefying dead tissue while leaving healthy cells completely untouched. This approach is far less invasive and painful than sharp debridement but acts more slowly, requiring consistent dressing changes over several days or weeks.
Autolytic Debridement: Your Body's Natural Cleanup Crew
This clever approach simply helps your body do what it does best. Autolytic debridement uses a special moisture-retentive dressing to create a moist environment around the wound. This moisture activates your body’s own enzymes, allowing them to soften and digest dead tissue naturally—much like letting a tough stain soak until it lifts away on its own. While it is highly selective and completely painless, it is also the slowest method. It's best suited for wounds with only a small amount of non-viable tissue and no signs of infection.
This infographic visualizes the specialized instruments used in sharp, mechanical, and enzymatic debridement, highlighting the precision required for each.
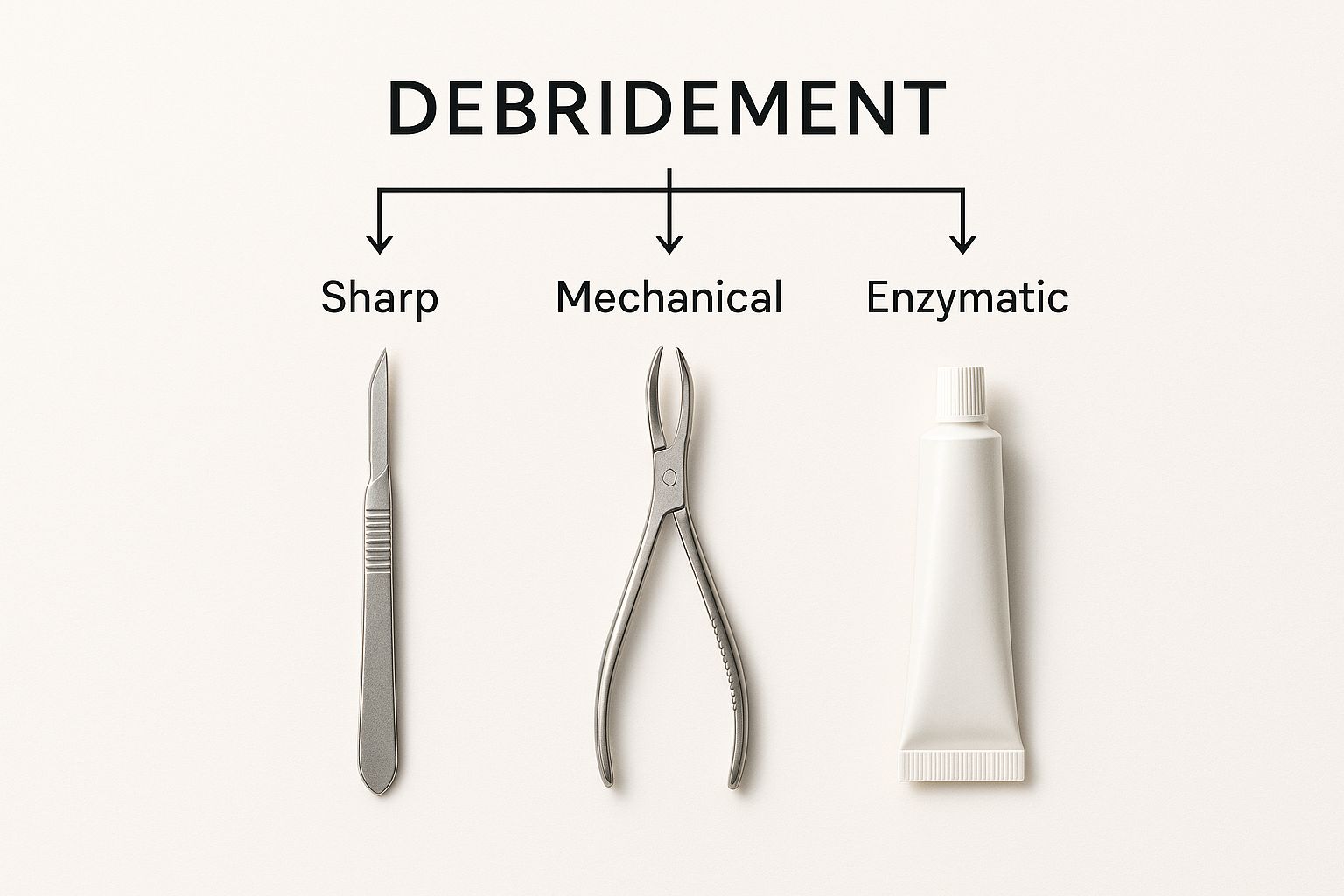
The image reinforces that a wound debridement procedure is a technical skill, with each tool designed for a specific type of tissue removal and level of invasiveness.
Mechanical Debridement: The Gentle Scrubber
Mechanical debridement works by physically clearing away dead tissue and debris from the wound bed, similar to gently scrubbing a stubborn spot. Common techniques include wound irrigation (using pressurized saline) or applying specialized gauze that lifts away loose material when removed. While it can be effective, a key consideration is that some mechanical methods are non-selective, meaning they might accidentally remove healthy tissue along with the unhealthy. The choice of debridement is heavily influenced by the wound itself. Learn more in our article about the different types of wounds to see why this connection is important.
Biological Debridement: Nature's Tiny Surgeons
Also known as larval therapy, this method enlists nature's most efficient cleanup crew: sterile, medical-grade maggots. These tiny creatures are placed on the wound under a dressing and get straight to work. They secrete enzymes that liquefy only dead tissue, which they then consume, leaving healthy tissue completely unharmed. As a bonus, they also help disinfect the wound. While the concept might make some people uneasy, this is an exceptionally precise and effective debridement method.
To help you understand how these methods compare, the table below offers a comprehensive comparison of the five main debridement methods, including their mechanisms, advantages, disadvantages, and typical applications.
| Debridement Type | Mechanism | Speed of Action | Pain Level | Best Used For | Contraindications |
|---|---|---|---|---|---|
| Sharp | Surgical removal with sterile instruments (scalpel, scissors). | Very Fast | High (may require anesthesia) | Large wounds, infected tissue, urgent situations. | Medically unstable patients, poor blood flow to the area. |
| Enzymatic | Topical ointment with enzymes dissolves dead tissue. | Moderate to Slow | Low to None | Wounds with moderate dead tissue; for patients unable to tolerate sharp debridement. | Allergy to the enzymes, use with certain metal-based products (e.g., silver). |
| Autolytic | Body's own enzymes break down tissue in a moist environment. | Very Slow | None | Non-infected wounds with minimal dead tissue. | Infected wounds, dry wounds, large amounts of dead tissue. |
| Mechanical | Physical force (irrigation, wet-to-dry dressings) removes debris. | Fast | Moderate to High | Wounds with loosely attached debris and foreign material. | Wounds with healthy granulation tissue, tightly adhered dead tissue. |
| Biological | Medical-grade maggots secrete enzymes to liquefy and consume dead tissue. | Moderate | Low | Non-healing wounds with dead tissue, especially when surgery isn't an option. | Allergy to maggots, deep wounds connecting to organs, severe infection. |
The key takeaway from this comparison is that there is no single "best" method. The right choice for a wound debridement procedure always depends on a careful and professional evaluation of the wound, the patient's overall health, and the specific goals of the treatment plan.
Recognizing When Your Wound Needs Professional Help
Knowing the difference between a minor healing delay and a serious problem is crucial for your recovery. Think of your body as trying to repair a road, but sometimes, debris gets in the way. Spotting this debris early tells you when it’s time to call in a professional road crew for a wound debridement procedure to clear the path.
The Warning Signs: When Healing Goes Wrong
A healthy wound should be clean and pink, slowly closing in on itself. When healing stalls, the wound sends out clear distress signals. These signs indicate that dead tissue or bacteria are creating roadblocks that your body can’t remove on its own. Watch for these critical red flags:
- Concerning Colors: Healthy tissue is red or pink. If you notice yellow, gray, tan, or black tissue, it’s a sign of non-viable tissue. These are known as slough (the yellowish, softer tissue) or eschar (the hard, black scab).
- Troubling Drainage: Some clear fluid is normal, but thick, cloudy, green, or brown drainage—also known as pus—is a clear indicator of infection.
- Foul Odor: A persistent, unpleasant smell from the wound, even after you’ve cleaned it, points to significant bacterial activity.
- Rolled Edges: If the skin at the wound’s border appears to be curling inward, a condition called epibole, it means the healing process has hit a wall. The new skin cells have nowhere to go.
- No Progress: A wound that hasn't gotten any smaller over 2-4 weeks is considered chronic. This is a major sign that it requires medical intervention to get back on track.
How Professionals See Your Wound: The Assessment Process
When you visit a wound care specialist, they do more than just a quick look. They conduct a thorough evaluation to understand exactly what’s happening. They will measure the wound, check the tissue type, and document every detail to build a complete picture of its condition.

Clinicians often use a framework like T.I.M.E. to guide them: Tissue (is it alive?), Infection/Inflammation (are there signs?), Moisture (is the balance right?), and Edge (are the borders advancing?). This detailed look helps them decide if a wound debridement procedure is the necessary next step.
To make this clearer, healthcare providers rely on specific criteria to judge a wound's status. The table below outlines what they look for when deciding if debridement is needed.
| Assessment Factor | Normal Healing | Requires Debridement | Urgency Level |
|---|---|---|---|
| Wound Color | Healthy pink or red tissue | Yellow, gray, tan, or black tissue (slough/eschar) | Medium to High |
| Drainage | Minimal, clear, or light yellow fluid | Thick, cloudy, green, or brown pus | High |
| Odor | No persistent or unpleasant smell | A foul, persistent odor | High |
| Wound Edges | Flat, attached, and migrating inward | Rolled inward (epibole) or detached from the wound base | Medium |
| Healing Progress | Gradually decreasing in size | No change or increase in size over 2-4 weeks | Medium to High |
This table shows that a combination of factors, especially a foul odor, concerning drainage, and non-viable tissue, signals a high-urgency situation where debridement is likely required to prevent serious complications.
Conditions That Increase the Need for Debridement
Certain health issues can slow down or interfere with the body's healing process, making professional debridement more common. If you have one of these conditions, it’s especially important to monitor any wounds closely.
- Diabetic Foot Ulcers: High blood sugar can cause nerve damage and poor circulation, so even a small cut on the foot can become a serious wound that struggles to heal.
- Pressure Injuries: Also known as bedsores, these wounds form when constant pressure on one area cuts off blood flow, causing the skin and underlying tissue to die.
- Venous Leg Ulcers: These are caused by poor blood flow in the leg veins and often produce a lot of fluid, creating a perfect environment for slough to form.
- Post-Surgical Wounds: Sometimes, a surgical incision can get infected or fail to close correctly. Debridement is then needed to clean the area so healing can restart.
Ignoring these warning signs isn't a "wait and see" situation—it's a risk. A delayed wound debridement procedure can allow an infection to spread, potentially leading to bone infections or sepsis. Seeking prompt care is vital. As studies show, effective home health wound care can lead to better patient outcomes by ensuring problems are caught and treated early. Being proactive is your best line of defense.
What Really Happens During Your Procedure
Walking into a medical appointment for a wound debridement procedure can feel intimidating. But understanding what's going to happen can turn that anxiety into confidence. Let's walk through the entire process, step by step, so you know exactly what to expect and can become an active partner in your own healing.
Getting Ready: Preparation and Comfort
Your comfort is the first thing your care team will address. Before the procedure begins, they will focus on making sure you feel as little as possible. This isn't something you just have to endure.
Depending on the wound and the type of debridement, your provider might apply a topical anesthetic (a numbing cream or gel). For deeper work, they may use a local anesthetic injection, much like the one you get before a dental filling, to completely numb the area.
The provider will also carefully clean the skin around the wound to prevent any new germs from getting in. The procedure itself can last anywhere from a few minutes to over an hour, depending on the wound's size and complexity. Your provider will give you a clear time estimate before they start.
The Main Event: What Your Provider Is Doing
Once the area is numb and clean, the debridement begins. This is a highly precise and controlled process. Think of a master gardener carefully pruning away dead branches to allow the healthy plant to flourish. Your provider is doing the same for your wound.
They methodically remove only the dead or unhealthy tissue and biofilm that are stopping your body from healing. Every piece of healthy tissue is carefully preserved.
You shouldn't feel pain, but you might notice sensations of pressure or gentle pulling. The goal is to keep you comfortable, so if you start to feel any real discomfort, it’s vital to speak up immediately. They can always adjust your pain management. Each bit of tissue removed clears the way for your body’s natural healing to begin.
Where the Healing Happens: Your Treatment Environment
A wound debridement procedure doesn’t always mean a trip to a hospital operating room. Many of these treatments are done in much more convenient and less intimidating settings.
Common locations include:
- A private procedure room in a doctor's office.
- A specialized outpatient wound care clinic.
- The comfort of your own home, with a visit from a trained specialist from a service like Rapid Wound Care.
These environments are designed to be safe, clinical, and reassuring. Specialized centers, like those operated by Healogics, are built specifically to provide advanced wound treatments in a comfortable setting.
The setting is a key part of making the experience feel positive and focused on your recovery.
Your Voice Matters: Communication Is Key
Your role in this process is crucial. You aren't just a patient; you are an essential member of the care team. The best results come from a strong partnership between you and your provider.
Don't be afraid to ask questions before, during, or after your treatment. Good questions to start with are:
- "What type of debridement will you be doing?"
- "What sensations should I expect to feel?"
- "Roughly how long will this procedure take?"
Most importantly, be your own advocate for comfort. Your provider depends on your feedback. If you feel pain, tell them. If you're nervous, let them know. They can offer more anesthetic, take a brief pause, or talk you through the process to ease your mind. This open dialogue ensures the procedure is effective and puts you on the best path to healing.
The Real Benefits And Honest Risks You Should Know

Any medical procedure comes with its own set of pros and cons, and a wound debridement procedure is no exception. Understanding both sides is the first step toward making an informed decision about your care. For a wound that has simply stopped getting better, this procedure can be the turning point that gets your body’s natural healing process back on track.
The Powerful Benefits of Clearing the Way
When a wound’s healing has stalled, the advantages of debridement are significant. Imagine trying to build a new foundation on a site cluttered with old debris; it just won't work. Debridement clears that debris so the real work can begin.
The primary benefits include:
- Kickstarting the healing process. By clearing away dead tissue and bacterial buildup, the procedure creates a clean, healthy base. This gives new, healthy cells the space and resources they need to grow and close the wound.
- Lowering the risk of infection. Dead, or necrotic, tissue is a perfect environment for harmful bacteria to thrive. Removing this tissue effectively starves out potential infections, preventing complications that could lead to more serious health issues.
- Improving the effectiveness of other treatments. Medicated ointments, advanced dressings, and other therapies work far better on a clean wound surface. Debridement essentially preps the wound to get the maximum benefit from the rest of your care plan.
Clinical data shows that removing non-viable tissue is a critical step in preparing a chronic wound for successful closure. You can explore the full research on wound healing outcomes to see the supporting evidence for yourself.
A Clear-Eyed View of the Potential Risks
An honest conversation about debridement also means looking at the potential downsides. The good news is that these risks are generally manageable and temporary.
Here’s what to be aware of:
- Minor bleeding and discomfort. It’s common to experience some soreness or minor bleeding after the procedure. This is often a good sign, as it shows that healthy blood is now flowing to the area, which is vital for healing. Your provider will ensure you have a pain management plan.
- Accidental removal of healthy tissue. This is a rare risk that is minimized by choosing an experienced provider. A skilled clinician can tell the difference between healthy and non-viable tissue and will select the most precise debridement method for your specific situation.
- Post-procedure infection. While debridement cleans the wound, it also leaves it open and vulnerable for a short time. This is why following your aftercare instructions is so important. Proper hygiene and dressing changes are your best defense against new infections, which is especially true for wounds like pressure ulcers. You can find more tips in our detailed guide on pressure ulcer treatment and at-home care.
For most non-healing wounds, the benefits of a wound debridement procedure strongly outweigh the manageable risks. Having this information helps you work with your healthcare team to make the best choice for your health and recovery.
Your Post-Procedure Success Roadmap
Completing a wound debridement procedure is a huge step forward, but the healing journey continues. Think of the procedure as clearing the way for new construction; your aftercare is the blueprint that guides the rebuilding process. Your commitment to this next phase is what ensures a strong, complete, and timely recovery.
What to Expect Immediately After Debridement
In the first few days, you'll see your body’s healing response kick into gear. It's normal for the wound area to be tender, slightly red, and have a small amount of clear or pinkish drainage. This is a positive sign that healthy blood flow is returning to the site. However, you need to know the difference between normal healing and signs that require a doctor's attention.
You should contact your healthcare provider immediately if you notice any of these warning signs:
- Pain that gets worse and is not controlled by your medication.
- A bad smell coming from the wound or dressing.
- Thick, cloudy, or green-colored fluid (pus) draining from the wound.
- Redness and warmth that spreads into the skin around the wound.
- A fever higher than 101°F (38.3°C).
Mastering Your At-Home Wound Care
After debridement, you become the day-to-day manager of your own healing. This means carefully following your provider’s directions for cleaning the wound and changing the dressing. This isn't just about keeping it clean; it’s about creating the perfect moist environment that helps new cells grow and repair the tissue.
The image below shows how successful home wound care is a team effort between you and your healthcare professional.
This partnership is essential. Consistent, expert-guided care at home leads to better healing and helps you avoid complications. Your dedication to this daily routine is the single most important factor for a successful outcome after your wound debridement procedure.
Building a Foundation for Long-Term Healing
To rebuild tissue, your body needs the right materials and conditions. This goes beyond just caring for the wound itself. Proper nutrition is a cornerstone of recovery. A diet high in protein, vitamins (especially A and C), and minerals like zinc gives your cells the building blocks they need. Drinking plenty of water to stay hydrated is just as important for healthy cell function.
Your provider will also give you specific instructions on your activity level. You may need to avoid putting pressure on the wound, but gentle movement can boost circulation, bringing oxygen and nutrients to the area. These habits are the foundation of a solid recovery, and you can find more tips in our guide to effective post-discharge wound care at home.
Finally, attending all your scheduled follow-up appointments is non-negotiable. These visits allow your provider to track your progress, adjust the care plan as needed, and make sure you’re on the path to a full recovery. This professional oversight helps catch small problems before they become serious setbacks.
Making Smart Financial Decisions About Your Care
A medical procedure can bring enough stress on its own without the added worry of a surprise bill. Getting a handle on the financial side of a wound debridement procedure gives you the power to make clear-headed decisions, so you can get the care you need without breaking your budget. It all comes down to knowing what to expect and which questions to ask.
Is a Wound Debridement Procedure Covered by Insurance?
For most patients, the short answer is yes. When a doctor determines that debridement is medically necessary to treat a wound that isn't healing, the procedure is generally a covered service. This applies to most major insurance plans as well as government programs like Medicare Part B. "Medically necessary" is simply the term used to confirm that a treatment is essential for your health, not just optional.
Most health insurance policies are designed to cover a wide array of benefits that directly support the wound healing process, as shown in this overview from HealthCare.gov.
This shows that core services like hospital care, prescription medications (like enzymatic debriding ointments), and rehabilitation are standard inclusions. This reinforces that a debridement your doctor orders is very likely to be covered. However, your specific out-of-pocket costs—your deductible, copayments, and coinsurance—will always depend on the details of your personal plan.
Factors That Influence Your Costs
The final bill for wound debridement isn't a single, fixed price. Several key factors can change what you ultimately pay:
- Type of Debridement: A complex surgical debridement that happens in an operating room will naturally cost more than an enzymatic or autolytic debridement that is managed with special dressings in a clinic.
- Treatment Setting: Where you receive care matters. Hospital-based procedures are typically the most expensive, followed by outpatient wound care clinics. At-home care from a mobile specialist is often a more convenient and cost-effective choice.
- Your Insurance Plan: The fine print of your policy, like your annual deductible, copay amounts, and coinsurance percentage, directly dictates your share of the bill after your insurance pays its part.
Proactive Steps to Avoid Billing Surprises
The best defense against a high medical bill is a good offense. Being proactive is key. Before scheduling your procedure, make time for a conversation with your provider’s billing office and your insurance company. Some treatments may require prior authorization, which means your insurer needs to approve it as necessary before you receive the care. Getting this approval upfront helps prevent a denied claim down the road.
Go into these conversations armed with a few essential questions:
- What is the estimated total cost of the debridement my doctor recommended?
- Is this procedure covered by my plan, and do I need to get prior authorization?
- After my insurance coverage, what will my estimated out-of-pocket cost be?
For anyone looking to balance costs with expert treatment, at-home services can be a fantastic option. Rapid Wound Care specializes in bringing advanced wound care directly to your home, a service often covered by plans like Medicare Part B. Contact us today to see how we can help.

