Understanding Bed Sores: What Every Caregiver Should Know
Proper treatment of bed sores depends on understanding what they are and why they develop. Bed sores, also called pressure ulcers or pressure injuries, occur when constant pressure on the skin restricts blood flow to the underlying tissues. This reduced circulation starves skin cells of oxygen and nutrients, leading to tissue breakdown and ulcer formation. This can happen quickly, often beginning as a slightly red area and progressing to a deep, painful wound. You might be interested in: How to master pressure ulcer treatment at home.
Risk Factors Beyond Immobility
While lack of movement is a primary risk factor, it's not the only one. Several conditions and external factors can increase a person's vulnerability to bed sores. For instance, people with diabetes often have reduced blood flow and nerve damage. This can make it difficult to feel pressure and hinder healing.
Malnutrition can also weaken the skin, making it more prone to breakdown. Some medications, like steroids, can thin the skin and increase the risk of pressure ulcers. Even environmental factors, such as excess moisture or friction from bedding, contribute to bed sore development.
Recognizing the Early Signs
Early detection of bed sores is vital for effective treatment. The first sign is often persistent redness that doesn't disappear when pressure is removed. This might be accompanied by skin temperature or texture changes. The affected area might feel warmer or cooler than the surrounding skin, or appear firmer or softer.
As the sore progresses, the skin may blister or break, forming an ulcer. In later stages, the wound might reach muscle, bone, or even tendons. The global prevalence of pressure ulcers is about 12.8%, with around 2.5 million cases treated annually in the United States. These sores primarily affect individuals with limited mobility, including those with chronic illnesses, disabilities, or older adults. Find more statistics here.
The Importance of Swift Action
Understanding the basics of bed sores—from causes to early signs—empowers caregivers to act quickly. This means implementing preventative measures and addressing developing sores promptly to minimize complications and encourage healing. This knowledge also helps caregivers communicate effectively with healthcare professionals, providing valuable information for a more comprehensive treatment plan.
Immediate Action Steps That Make a Real Difference
When you discover a bed sore, taking swift action is vital for effective treatment. This section outlines the essential first steps recommended by wound care professionals, starting with pressure relief and ending with accurate documentation for healthcare providers. These initial actions can significantly impact healing and minimize potential complications.
Relieving Pressure: The First Line of Defense
The most immediate step in treating a bed sore is to alleviate the pressure causing it. This involves repositioning the individual every two hours to distribute weight evenly. For instance, if a sore develops on the tailbone, shifting the person onto their side can relieve pressure and improve blood flow to the affected area. Use pillows or specialized cushions to elevate and support vulnerable areas, such as heels and elbows. This prevents further tissue damage and promotes healing.
Cleaning and Protecting the Wound
Proper wound care is crucial to prevent infection and encourage healing. Clean the bed sore gently with mild soap and water, or a saline solution. Avoid harsh chemicals or scrubbing, which can irritate the wound. After cleaning, gently pat the area dry and apply a sterile dressing. This protects the wound and helps maintain a moist environment essential for tissue regeneration.
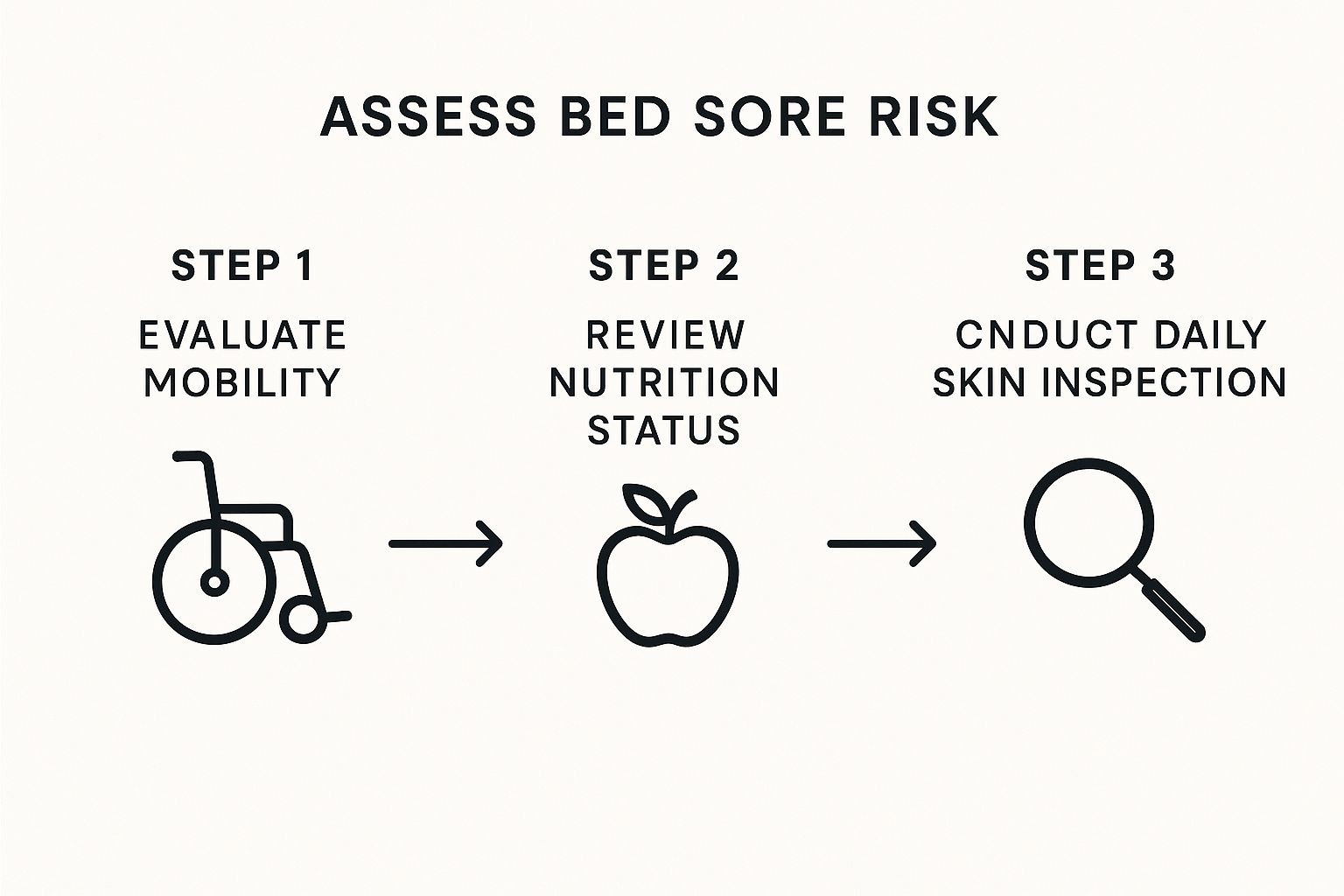
This infographic highlights three key steps for assessing bed sore risk: evaluating mobility, reviewing nutritional status, and conducting daily skin inspections. By addressing these factors, caregivers can proactively minimize the risk of bed sores. Regular monitoring and preventative measures are especially important for individuals with limited mobility or poor nutrition.
Assessing Wound Severity: Knowing When to Seek Professional Help
Accurately assessing the severity of the bed sore is crucial for determining the right course of action. Visual cues like the size and depth of the wound offer valuable information. Also, check for signs of infection, including pus, redness, swelling, or a foul odor. If the sore is deep, involves muscle or bone, or shows signs of infection, seek immediate medical attention. Prompt professional intervention is essential for complex or infected bed sores to prevent serious complications.
The following table summarizes the stages of bed sores, their appearance, and the immediate actions required.
Bed Sore Stage Assessment and Initial Treatment
| Stage | Appearance | Immediate Action | Medical Urgency |
|---|---|---|---|
| Stage 1 | Reddened skin that does not blanch (turn white) when pressed. | Relieve pressure, keep clean and dry. | Monitor closely. |
| Stage 2 | Partial-thickness skin loss involving the epidermis and/or dermis. May look like a blister or abrasion. | Relieve pressure, clean with saline, apply sterile dressing. | See a healthcare professional. |
| Stage 3 | Full-thickness skin loss involving damage or necrosis of subcutaneous tissue. May extend down to, but not through, underlying fascia. | Relieve pressure, clean with saline, apply appropriate dressing, consider advanced wound care modalities. | Urgent medical attention required. |
| Stage 4 | Full-thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures. | Relieve pressure, protect the wound, seek immediate medical intervention. | Immediate medical attention required. |
This table provides a quick guide for initial assessment and action. Remember, accurate staging requires professional evaluation.
Managing Pain and Discomfort
Bed sores can be painful, so managing discomfort is a key aspect of treatment. Over-the-counter pain relievers like ibuprofen or acetaminophen can help reduce pain and inflammation. Always consult a healthcare professional before using any medication, particularly if the individual has other health conditions. Minimizing friction and shear forces during repositioning is also important. Use proper lifting techniques and assistive devices to avoid dragging the skin.
Documenting Your Observations: A Crucial Step for Effective Care
Detailed records of your observations are essential for effective communication with healthcare providers. Note the size, depth, and appearance of the sore, along with any changes. Documenting pain levels, treatments given, and the individual's overall condition provides valuable information. This documentation helps healthcare professionals track progress, adjust treatment, and ensure optimal healing.
Professional Treatments That Accelerate Healing
Beyond basic wound care, a range of professional treatments can significantly improve healing outcomes for bed sores. These treatments target the underlying causes and encourage faster, more effective healing.
Specialized Dressings: Creating the Optimal Healing Environment
The right dressing is crucial for effective bed sore treatment. For example, hydrocolloid dressings create a moist, protective environment that promotes cell growth and minimizes pain. Foam dressings absorb excess fluid and shield the wound from further pressure. Antimicrobial dressings help prevent infection in wounds that are already contaminated. The specific dressing is chosen based on the wound's characteristics, including its size, depth, and the amount of fluid it produces. You might be interested in: How to master deep wound healing.

Debridement: Removing Barriers to Healing
Dead or damaged tissue can sometimes hinder the healing process. Debridement, the removal of this unhealthy tissue, creates a clean wound bed for healthy tissue to grow. Several methods exist, including surgical, enzymatic, autolytic, and mechanical debridement. The best method depends on the wound's condition, the patient's overall health, and the available resources.
Infection Control: Addressing a Common Complication
Infection is a serious concern with bed sores. If a wound becomes infected, antibiotics may be necessary to control the infection and prevent further complications. Oral antibiotics are sometimes sufficient, but intravenous antibiotics might be required in more severe cases. Infected wounds require meticulous care and frequent monitoring to ensure the infection is healing effectively.
Advanced Therapies: Accelerating the Healing Process
For complex or slow-healing bed sores, advanced therapies can be incredibly beneficial. Negative pressure wound therapy (NPWT) uses a vacuum device to remove fluid and stimulate blood flow to the wound. This speeds up healing, reduces infection risk, and can even decrease the wound's size.
Emerging Therapies: Exploring New Frontiers in Wound Healing
Emerging therapies offer new hope for treating challenging bed sores. Growth factors are proteins that stimulate cell growth and repair. These can be applied topically to enhance healing. Bioengineered skin substitutes provide a temporary covering, promoting healing and minimizing scarring. These advanced treatments, while promising, require careful consideration and discussion with a healthcare professional.
Surgical Interventions: For Complex or Non-Healing Cases
Sometimes, surgical intervention is necessary to treat bed sores. Surgery can remove infected tissue, improve blood flow, or close large wounds. Skin grafts, where healthy skin is transplanted to cover the wound, are sometimes performed for extensive or deep bed sores. This procedure facilitates wound closure and reduces further complications. While surgery has risks, it can be life-saving for severe bed sores. Surgical treatments are typically considered after other therapies have been unsuccessful.
The best treatment for bed sores depends on several factors, including the wound's stage, the patient's overall health, and available resources. A comprehensive treatment plan should address not only the wound itself but also underlying risk factors like malnutrition and immobility. Regular wound reassessment and adjustments to the treatment plan are essential for optimal healing.
Home Care Strategies That Actually Work
Effective home management of bed sores, also known as pressure ulcers, is essential for healing and preventing complications. This guide offers practical strategies from experienced caregivers and home health professionals, providing insights into effective home care.
Positioning Techniques for Pressure Relief
Relieving pressure on the affected area is fundamental to home care for bed sores. This involves regular repositioning, ideally every two hours, to distribute weight and restore blood flow. For instance, if a sore is on the tailbone, repositioning onto the side can help. Use pillows or cushions to support vulnerable areas like heels and elbows. Learn more in this helpful article: How Home Wound Care Speeds Up Recovery.

Turning Schedules and Rest
A structured turning schedule is crucial, balancing pressure relief with rest. A chart can track repositioning times and ensure consistency. The schedule should be personalized to the individual's comfort and tolerance. Consistent care is key, but avoid disrupting the healing process.
Skin Inspection: Catching Problems Early
Regular skin inspections are vital for early detection. Carefully examine the skin, focusing on bony prominences and pressure-prone areas. Look for redness, discoloration, or texture changes. Early detection allows for prompt intervention, preventing minor irritation from becoming a serious ulcer.
Creating a Healing Environment
The environment plays a crucial role in healing. Proper ventilation regulates temperature and humidity, preventing excess moisture. Temperature control is also essential, as extremes can hinder healing. A comfortable room temperature promotes tissue repair.
Pressure-Relieving Devices: Selection and Use
Various pressure-relieving devices can help. These include specialized mattresses, cushions, and overlays designed to distribute weight. Selecting the right device depends on individual needs and sore location. Proper use maximizes effectiveness and ensures comfort.
Safe Transfer Techniques: Protecting Vulnerable Skin
Transferring individuals with bed sores requires careful attention. Use proper lifting techniques and assistive devices like transfer boards or mechanical lifts to avoid friction and shear forces that can worsen sores.
Developing Sustainable Daily Care Routines
A sustainable daily care routine is key for long-term success. This should encompass all aspects of bed sore management, from repositioning and skin care to wound cleaning and dressing changes. Tailor the routine to individual needs and resources, making it manageable for both patient and caregiver. This ensures consistent care and prevents caregiver burnout.
Nutrition and Lifestyle Factors for Faster Recovery

Nutrition plays a crucial role in bed sore treatment and the overall healing process. Proper nutrition gives the body the necessary building blocks for tissue repair and a robust immune response. This means adequate nutrition can significantly impact how quickly and effectively bed sores heal.
The Power of Protein, Vitamins, and Minerals
Protein is vital for building and repairing tissues, making it a cornerstone of bed sore treatment. Getting enough protein helps rebuild damaged skin and encourages new cell growth. In addition, certain vitamins and minerals are essential for wound healing. Vitamin C, for example, is crucial for producing collagen, a key component of skin and connective tissue. Zinc also plays a significant role in cell growth and repair. A balanced diet rich in these nutrients is vital for faster healing.
Ensuring patients receive these essential nutrients is key to their recovery. This can be achieved through careful meal planning and consideration of individual needs and challenges.
Practical Meal Planning for Bed Sore Patients
Sometimes, incorporating these essential nutrients into a patient's diet can be difficult, especially if they have a poor appetite or have trouble swallowing. Offering smaller, more frequent meals packed with nutrient-rich foods can be easier to manage than three large meals. Smoothies, soups, and pureed foods can be simpler to consume while still delivering necessary nutrition. Adjusting mealtimes to fit around medications or other treatments can also improve nutrient absorption.
The following table provides a helpful overview of essential nutrients and their role in bed sore healing. It also lists daily requirements and good food sources for each nutrient.
Essential Nutrients for Bed Sore Healing: Key nutrients, their healing benefits, and food sources for optimal wound recovery
| Nutrient | Healing Benefit | Daily Requirement | Food Sources |
|---|---|---|---|
| Protein | Builds and repairs tissues | 0.8 grams per kilogram of body weight | Meat, poultry, fish, eggs, beans, lentils, tofu, dairy products |
| Vitamin C | Essential for collagen production | 75-90 mg | Citrus fruits, berries, tomatoes, peppers |
| Zinc | Supports cell growth and repair | 8-11 mg | Meat, shellfish, nuts, seeds, legumes |
| Vitamin A | Supports skin health and immune function | 700-900 mcg | Sweet potatoes, carrots, spinach, kale |
| Vitamin D | Aids calcium absorption and bone health | 600-800 IU | Fatty fish, fortified milk, egg yolks |
This table highlights the importance of a balanced diet rich in these key nutrients. It provides a practical guide for caregivers and patients aiming to optimize their nutritional intake for faster healing.
Overcoming Common Nutritional Challenges
Several factors can complicate nutritional management for bed sore patients. Some medications can interact with nutrient absorption, hindering the body's ability to utilize essential nutrients. Dietary restrictions, like allergies or intolerances, can also add another layer of complexity to meal planning. For caregivers managing nutrition for bed-bound individuals, finding practical solutions is crucial. Consulting a registered dietitian or nutritionist can be invaluable. They can help develop a personalized meal plan addressing individual needs and challenges. You might be interested in: Windy City Wound Care's Knowledge Base.
Supplements and Lifestyle Modifications
While a healthy diet is the primary source of nutrients, certain supplements can aid healing. For instance, Vitamin D supplementation might be helpful, especially for individuals with limited sun exposure. However, it's crucial to consult a healthcare professional before starting any new supplements to avoid potential interactions with current medications.
Lifestyle modifications, such as quitting smoking and managing underlying conditions like diabetes, also contribute to faster recovery. Smoking impairs blood circulation, which hinders the delivery of oxygen and nutrients to the wound. Effectively managing diabetes helps maintain healthy blood sugar levels, which further optimizes wound healing. These lifestyle changes, combined with nutritional adjustments, significantly support and accelerate bed sore recovery.
Prevention Strategies That Stop Problems Before They Start
Preventing bed sores is always the best course of action, particularly for individuals at increased risk. This section details comprehensive prevention strategies employed by healthcare professionals in long-term care settings. These strategies prioritize proactive measures to maintain skin health and minimize contributing risk factors.
Positioning Schedules: Balancing Pressure and Comfort
Regular repositioning is vital for bed sore prevention. This involves changing a person's position every two hours to alleviate pressure on vulnerable areas. However, repositioning shouldn't compromise comfort.
Using pillows and wedges can support proper alignment and enhance comfort during repositioning. This balance ensures pressure relief while prioritizing patient well-being. Read also: Wound Care in Chicago Delivered.
Skin Care Routines: Maintaining Integrity Without Irritation
Healthy skin is a cornerstone of bed sore prevention. This involves keeping the skin clean and dry, especially in areas prone to moisture buildup.
Gentle cleansing with mild soap and water, followed by thorough drying, helps prevent skin breakdown. Avoid harsh chemicals or aggressive scrubbing, which can damage the skin and elevate the risk of sores. Moisturizing dry skin with lotions or creams also helps maintain skin integrity.
Environmental Modifications: Reducing Risk Factors
The environment plays a significant role in bed sore prevention. This includes ensuring adequate ventilation to regulate temperature and humidity, preventing excessive moisture. Maintaining a comfortable room temperature is also important.
Consider specialized mattresses, cushions, or overlays designed to distribute pressure evenly. These modifications create a supportive environment that minimizes risk. Minimizing friction during movement is also crucial. Using proper lifting techniques and assistive devices can prevent skin damage.
Regular Skin Assessments: Early Detection and Intervention
Regular skin assessments are essential for early detection of potential issues. This involves careful examination of the skin, particularly over bony prominences, for any signs of redness, discoloration, or textural changes.
This vigilant approach enables prompt intervention, addressing minor irritations before they progress into bed sores. Early intervention is generally easier and more effective than treating established ulcers. The number of bed sore cases globally has increased considerably, from 300,442 in 1990 to 645,588 in 2021, reflecting factors like the aging global population. Explore this topic further here.
Caregiver Education: Empowering Effective Care
Educating family members and caregivers about bed sore prevention is paramount. Sharing best practices and demonstrating proper techniques empowers them to provide consistent, quality care.
This includes instruction on repositioning, maintaining skin hygiene, and recognizing early warning signs. This shared responsibility promotes vigilant care and lessens the burden on individual caregivers. This proactive approach helps prevent bed sores, fostering collaboration to maintain skin health and overall well-being.
When to Seek Help and What to Expect During Recovery
Knowing when to seek professional help for a bed sore is crucial to prevent serious complications. While some bed sores can be managed at home, others require immediate medical intervention. This section offers guidance on recognizing warning signs, understanding healing timelines, and navigating the healthcare system for optimal bed sore treatment.
Recognizing Warning Signs: When to Seek Immediate Medical Attention
Early-stage bed sores can often be treated at home. However, certain symptoms indicate the need for immediate medical attention.
-
Signs of Infection: If you notice pus, increased redness or swelling around the sore, a foul odor, or if the patient develops a fever, seek immediate medical evaluation. Infection can rapidly worsen and spread, leading to serious health risks.
-
Rapidly Expanding Sores: A bed sore that increases quickly in size or depth may necessitate specialized treatment. This will help control its progression and prevent further tissue damage.
-
Deep or Extensive Tissue Damage: If the sore extends into the muscle, bone, or tendons, professional wound care is essential. This might involve specialized dressings, debridement, or even surgery.
-
Intense Pain: Uncontrolled pain, even with over-the-counter pain relievers, indicates a need for professional intervention. Healthcare providers can recommend stronger pain relief options and address underlying issues causing discomfort.
These warning signs suggest the bed sore may be progressing or becoming infected, requiring prompt medical evaluation and treatment.
Understanding Healing Timelines and Setting Realistic Expectations
Healing times for bed sores differ based on the stage of the sore and the individual's overall health. Stage 1 sores, characterized by redness, might heal within a few days or weeks with proper pressure relief and care. Deeper sores, especially those involving tissue damage, can take several weeks or even months to heal completely. Factors like nutrition, underlying health conditions, and consistent care also affect healing. A healthcare professional can provide a more accurate estimate based on the individual's specific situation.
Communicating With Healthcare Providers and Advocating for Optimal Care
Clear communication with healthcare providers is essential for successful treatment. This involves providing detailed information about the sore's development, pain levels, and any at-home treatments administered. Asking questions about treatment options, expected outcomes, and potential complications helps ensure everyone is on the same page. For instance, inquiries about specific dressing types or pain management strategies can lead to a more informed treatment approach.
If you feel your concerns aren't being addressed, advocate for the patient's needs. This might involve seeking a second opinion or requesting a referral to a wound care specialist. Open communication empowers you to participate actively in the patient's care and ensure they receive the best possible treatment.
What to Expect During Medical Consultations and Discharge Planning
During a consultation, the healthcare provider will assess the sore's stage, size, depth, and any signs of infection. They may take photographs or measurements to track its progress. Be prepared to discuss your home care routine, including repositioning techniques and wound cleaning methods. Ask questions about recommended treatments and potential side effects.
Discharge planning should include clear instructions on wound care, pain management, and follow-up appointments. Ensure you understand how to change dressings, recognize signs of infection, and adjust the care plan as needed. A detailed discharge plan ensures a smooth transition from the hospital or clinic to home and promotes continued healing.
Building a supportive healthcare team, which may include nurses, physical therapists, and dietitians, is essential for ongoing management and monitoring. This collaborative approach ensures comprehensive care addressing all aspects of bed sore treatment and prevention.
For comprehensive at-home wound care, consider Rapid Wound Care. Their certified professionals provide personalized treatment plans tailored to individual needs, ensuring optimal outcomes for bed sores and other complex wounds.

