The Hidden Crisis: Understanding Diabetic Foot Ulcers

Diabetic foot ulcers present a serious complication of diabetes, often developing from minor injuries. This occurs due to the physiological changes diabetes causes in the body. High blood sugar levels, for instance, can damage blood vessels and nerves, especially in the feet. Consequently, even small cuts or blisters can heal slowly and become infected.
The Role of Nerve Damage and Poor Circulation
Peripheral neuropathy, or nerve damage, is one of the most concerning aspects of diabetic foot ulcers. It can lead to a loss of feeling in the feet, meaning a developing ulcer might go unnoticed. Diabetes also often causes poor circulation, which further hinders the healing process. This dangerous combination makes it easy for ulcers to form and worsen without the patient’s awareness.
Untreated ulcers can rapidly develop into severe infections. This can lead to serious consequences, including osteomyelitis (bone infection) and even amputation.
The Global Impact of Diabetic Foot Ulcers
Diabetic foot ulcers (DFUs) are a significant global health concern, affecting approximately 18.6 million people annually. This condition carries high morbidity and mortality rates. Mortality after DFU development reaches 5% in the first year and about 42% within five years.
Standard Treatment and Its Challenges
Standard treatment for DFUs involves surgical debridement to remove dead tissue, maintaining a moist wound environment with dressings, off-loading pressure from the affected foot, vascular assessment, infection control, and blood sugar management. A multidisciplinary diabetic foot wound clinic often coordinates these interventions.
Despite advancements in DFU care, healing outcomes remain suboptimal. This underscores the need for continued research into additional therapies that can improve healing times and reduce amputation rates.
The Economic Burden
The economic burden of DFUs is substantial. DFU treatment accounts for nearly one-third of all diabetic care costs. In the United States alone, direct healthcare expenses for diabetes reached $176 billion. This emphasizes the clinical severity and significant financial impact of diabetic foot ulcers worldwide. More detailed statistics can be found here: Diabetic Foot Ulcers Statistics.
Recognizing the Warning Signs
Early detection is critical for preventing serious complications. While pain might be absent due to nerve damage, other warning signs should never be ignored.
- Changes in skin color (redness, darkening)
- Swelling or inflammation around a wound
- Drainage or unusual odor
- Formation of calluses or thickened skin
Any of these signs require immediate medical attention. Learn more about treatment in this article: Treating Diabetic Foot Ulcers. Recognizing these red flags early and seeking prompt care is vital for effective treatment. Addressing these issues proactively can significantly improve healing outcomes and prevent severe consequences.
Your Home Healing Toolkit: Essential Treatment Foundations
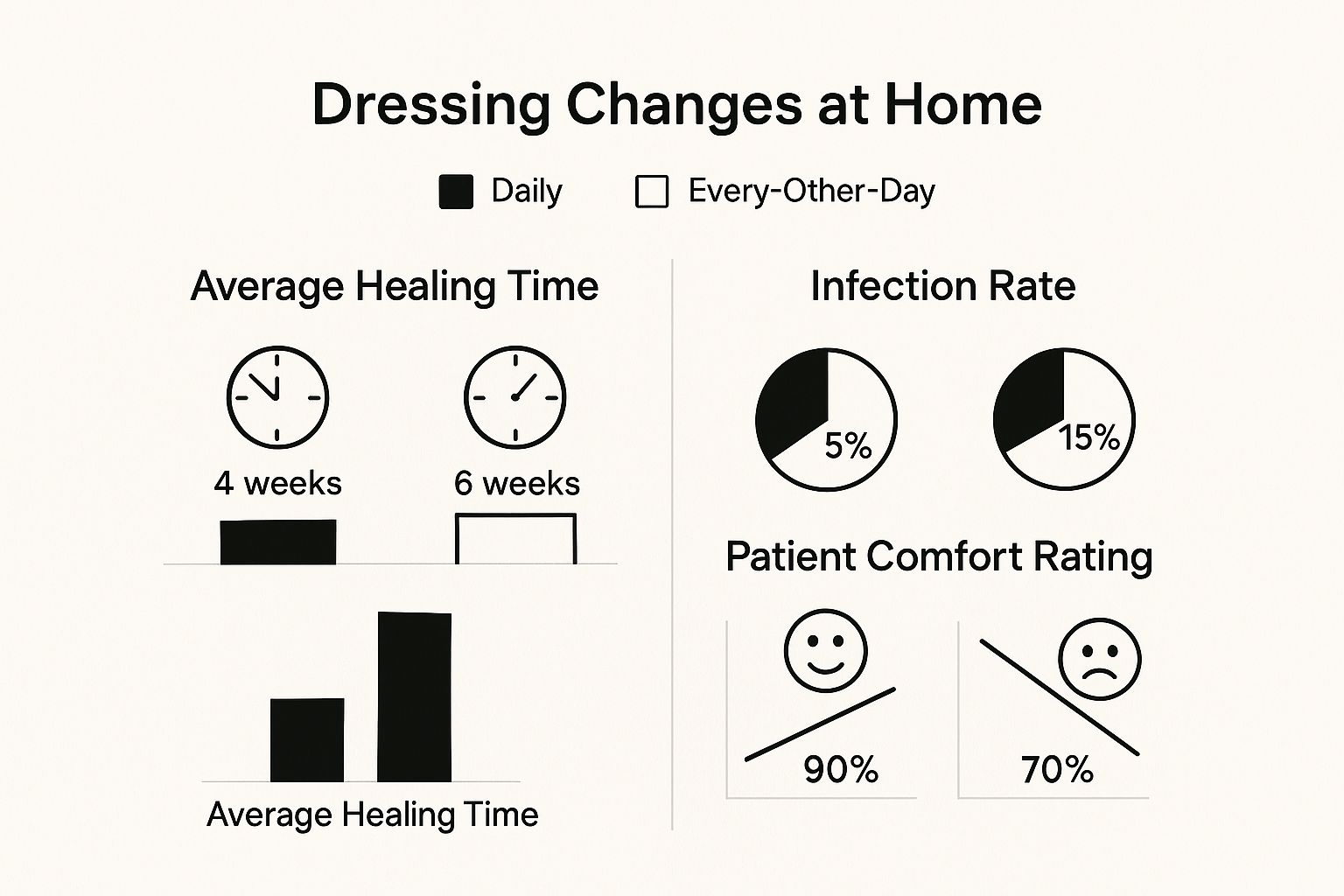
This infographic illustrates the difference between daily and every-other-day dressing changes for diabetic foot ulcer treatment at home. The results clearly show daily changes lead to significantly improved outcomes. Healing time is reduced (4 weeks vs. 6 weeks), infection rates are lower (5% vs. 15%), and patient comfort is higher (90% vs. 70%). This underscores the importance of consistent and appropriate wound care in the home.
Cleansing the Wound: A Gentle Approach
Effective at-home treatment for diabetic foot ulcers starts with proper cleansing. Think of the wound bed as delicate, needing debris removed without disrupting new tissue growth. Normal saline solution is the generally recommended cleanser due to its gentle nature, preventing harm to healing tissue. Avoid harsh antiseptics or home remedies like hydrogen peroxide, which can actually slow down the healing process.
Maintaining Optimal Moisture: The Goldilocks Principle
Wound moisture needs to be balanced – not too wet, not too dry. Excessive moisture can cause maceration, where the surrounding skin softens and breaks down. On the other hand, a dry wound can impede new tissue growth. The goal is a slightly moist environment that promotes healing. Specialized dressings like hydrocolloids or hydrogels can help achieve this balance. You may find helpful information in this article: How to master deep wound healing.
Offloading Pressure: Giving Your Foot a Break
One of the most important elements of home treatment is offloading, meaning relieving pressure from the ulcer. Just like resting a sprained ankle, reducing pressure is crucial for healing. This can involve specialized footwear, crutches, or custom orthotics. Minimizing pressure, even from everyday activities like walking, allows the ulcer to heal undisturbed.
Dressing the Wound: Choosing the Right Protection
Selecting the right dressing is another key step. Different dressings have various functions, from absorbing excess moisture to creating a protective barrier. Your healthcare provider can recommend the most appropriate dressing type based on your specific ulcer. Regular dressing changes, as advised by your doctor or wound care specialist, prevent infection and promote healing.
Monitoring and Follow-Up: Staying Ahead of Complications
Regularly monitoring your diabetic foot ulcer is crucial. Look for signs of infection like increased pain, swelling, redness, or a foul odor. Contact your healthcare provider immediately if you notice any of these. Consistent follow-up appointments are also vital to assess healing progress and adjust your treatment plan as needed.
The following table provides a comparison of various cleaning solutions for diabetic foot ulcers, considering their effectiveness, suitability for home use, cost, and safety.
Diabetic Foot Ulcer Cleaning Solutions Comparison
| Cleaning Solution | Effectiveness | Home Use Suitability | Cost | Safety Considerations |
|---|---|---|---|---|
| Normal Saline | High | Excellent | Low | Very Safe |
| Sterile Water | Moderate | Excellent | Low | Very Safe |
| Povidone-Iodine (low concentration) | High | Moderate | Moderate | Can irritate skin if used excessively |
| Hydrogen Peroxide | Low (can damage tissue) | Moderate | Low | Not recommended for long-term use |
| Wound Cleansers (commercial) | Varies | Varies | Moderate to High | Varies, consult with healthcare provider |
As shown in the table, normal saline and sterile water are generally preferred for home use due to their safety and effectiveness. While other options exist, they may have drawbacks and should be used under the guidance of a healthcare provider. Always consult with your doctor or wound specialist for personalized recommendations.
Breakthrough Technologies Transforming Home Ulcer Care

Beyond the basics of diabetic foot ulcer home treatment, exciting new technologies are changing how we approach care. These advancements bring professional-level treatment into the comfort of your home, making managing diabetic foot ulcers more effective.
Advanced Dressings: Optimizing The Healing Environment
One significant advancement is the development of advanced wound dressings. These dressings go beyond basic protection to actively promote healing. Hydrocolloids, for example, create a moist environment that encourages new tissue growth. Specialized foams offer cushioning and absorb extra fluid. This variety allows for personalized treatment based on individual needs.
Portable Negative Pressure Therapy: Accelerating Healing At Home
Negative Pressure Wound Therapy (NPWT), once limited to hospitals, is now available for home use. Portable NPWT devices, such as the RENASYS EDGE system, promote faster healing. They remove excess fluid and improve blood flow to the wound. This empowers individuals to benefit from advanced therapy at home. You can learn more about the benefits of home wound care: How home wound care speeds up recovery.
Monitoring Technologies: Early Detection And Intervention
Innovative monitoring technologies are also transforming home ulcer care. Some systems use sensors to detect subtle temperature or pressure changes. This allows for early detection of potential problems before they become visible, enabling timely intervention and preventing complications. Combining these technologies with Home Health Care for Seniors can further enhance your treatment plan.
Telehealth: Connecting Patients And Specialists Remotely
Telehealth platforms connect patients and specialists remotely. Through video calls and secure messaging, individuals can consult with healthcare providers without frequent in-person visits. This improves access to expert advice and streamlines communication, making home treatment more effective.
Home treatment for diabetic foot ulcers is benefiting from new technologies and advanced products. The global market for diabetic foot ulcer treatment was valued at approximately USD 8.33 billion in 2023. Projections estimate it will reach USD 14.37 billion by 2032. This growth reflects a shift from traditional methods to advanced dressings that optimize moisture control. Portable devices, enabling real-time monitoring, are becoming essential for home-based care. These innovations address the limitations of conventional treatments, which often lack continuous monitoring and can lead to complications. Learn more about this growing market: Diabetic Foot Ulcer Market Growth.
Healing From Within: Nutrition's Powerful Role
Meticulous wound care is crucial for treating diabetic foot ulcers at home. However, your body's internal environment is just as important for the healing process. Proper nutrition plays a powerful role in recovery. Just as a building needs a strong foundation, your body needs the right nutrients to rebuild damaged tissue.
The Building Blocks of Healing: Essential Nutrients
Specific nutrients are the building blocks for tissue regeneration and immune function. Protein, for example, is essential for cell repair and growth. Vitamin C helps produce collagen, a key component of skin and connective tissue. Zinc supports immune function and wound healing. These nutrients are fundamental to recovering from diabetic foot ulcers.
- Protein: Supports cell repair and growth. Excellent sources include lean meats, fish, eggs, and beans.
- Vitamin C: Crucial for collagen production. Find it in citrus fruits, berries, and leafy greens.
- Zinc: Supports immune function and wound healing. Good sources include nuts, seeds, and whole grains.
Blood Sugar and Healing: A Critical Connection
Maintaining healthy blood sugar levels is paramount for healing. High blood sugar impairs circulation and weakens the immune system. This makes it harder for your body to fight infection and rebuild damaged tissue. It’s like trying to put out a fire with a leaky hose. High blood sugar hinders your body’s ability to deliver essential resources to the wound site. Effective diabetic foot ulcer home treatment depends on managing blood sugar.
Identifying and Addressing Nutritional Deficiencies
Nutritional deficiencies can complicate healing. Many individuals with diabetes have deficiencies in Vitamin D, Vitamin B12, and iron. These nutrients are vital for overall health and wound recovery. Addressing these deficiencies through dietary adjustments or supplements can create a more supportive environment for healing.
Practical Nutrition Strategies: Incorporating Healing Foods
Making healthier food choices doesn't have to be overwhelming. Simple adjustments can make a big difference. Adding a handful of nuts to your breakfast provides healthy fats and zinc. Swapping white bread for whole-wheat bread increases your fiber intake and aids blood sugar control. Incorporating more fruits and vegetables into your meals boosts vitamin and mineral intake.
The following table details essential nutrients for diabetic foot ulcer healing. It outlines their benefits, food sources, and recommended intake. Consult a healthcare professional or registered dietitian for personalized recommendations.
Key Nutrients for Diabetic Foot Ulcer Healing:
| Nutrient | Role in Wound Healing | Food Sources | Recommended Daily Intake |
|---|---|---|---|
| Protein | Supports cell repair and growth | Lean meats, fish, eggs, beans, nuts | Varies based on individual needs |
| Vitamin C | Crucial for collagen production | Citrus fruits, berries, leafy greens | 75-90 mg |
| Zinc | Supports immune function and wound healing | Nuts, seeds, whole grains | 8-11 mg |
| Vitamin D | Supports bone health and immune function | Fatty fish, fortified milk, egg yolks | 600-800 IU |
| Vitamin B12 | Supports nerve function and red blood cell production | Meat, poultry, fish, eggs, dairy | 2.4 mcg |
| Iron | Carries oxygen to tissues | Red meat, poultry, fish, beans, leafy greens | Varies based on individual needs |
By prioritizing nutrition as part of your diabetic foot ulcer home treatment, you actively support your body's ability to heal. Remember, effective healing comes from both external care and internal nourishment. For further guidance on improving your gut health through nutrition, check out this resource: How to heal your gut. It emphasizes the vital role of gut health for optimal nutrient absorption and overall well-being.
Breaking the Cycle: Preventing Recurrence and Complications
Successfully treating a diabetic foot ulcer is a major step forward. But the journey to foot health doesn't stop there. Unfortunately, diabetic foot ulcers have a high rate of recurrence. In fact, about 65% of patients experience a recurrence within 3 to 5 years Find more detailed statistics here. This underscores the importance of prevention strategies.
Daily Foot Inspections: Your First Line of Defense
One of the most effective prevention methods is the daily foot inspection. This simple practice involves carefully checking your feet each day for any signs of change, no matter how minor they may seem.
- Look: Examine your feet for any cuts, blisters, redness, swelling, or changes in skin color.
- Feel: Run your hands over your feet to check for warm areas, tenderness, or any unusual textures.
- Use a mirror: If you struggle to see the bottoms of your feet, a mirror can be helpful. Alternatively, ask a family member to assist you.
Early detection is crucial. A small blister, if left unchecked, can quickly escalate into a serious ulcer, especially with the added challenges of reduced circulation and nerve damage often associated with diabetes.
Footwear: Choosing Protection and Support
Proper footwear is paramount in preventing diabetic foot ulcers. Shoes that fit correctly and provide ample support can significantly reduce pressure points and friction. This is especially important for individuals with diabetes, as even minor pressure can lead to skin breakdown and ulcer formation. Steer clear of shoes that are too tight, have rough seams, or high heels. For more information on foot care, check out this resource: How to master pressure ulcer treatment at home.
Integrating Preventative Care Into Your Routine
Making preventative care a daily habit might sound overwhelming, but it can be easily incorporated into your routine. Set aside a specific time each day for your foot inspection, perhaps after showering or before going to bed. Make it as routine as brushing your teeth. Also, be mindful of your footwear choices throughout the day. Prioritize comfort and support, even for casual wear.
The Balance of Self-Management and Professional Monitoring
While self-management is essential, regular check-ups with your healthcare provider are equally important. They can assess your overall foot health, identify potential issues, and adjust your diabetic foot ulcer home treatment plan if necessary. Combining diligent self-care with professional guidance is the most effective way to prevent recurrence and complications. Nutrition also plays a role in overall health. Learning more about gut health might be beneficial: how to heal your gut. Remember, managing diabetes and preventing foot ulcers is an ongoing commitment. The lifetime risk of developing a foot ulcer for someone with diabetes is estimated to be between 19% and 34%, highlighting the need for consistent, proactive care to maintain long-term foot health.
Red Flags: When Home Treatment Isn't Enough

While home treatment can be effective for managing minor diabetic foot ulcers, knowing when to seek professional help is crucial. This can literally save your limb, and potentially your life. This section highlights critical warning signs that demand immediate medical attention.
Recognizing the Signs of Infection
Even with meticulous home care, infections can still develop. Due to nerve damage associated with diabetes, pain may not be a reliable indicator. Instead, look for visual cues like increased redness, swelling, and warmth around the ulcer.
A change in the color or amount of drainage, especially if it becomes thick, cloudy, or foul-smelling, is a serious red flag. If you notice any of these changes, contact your doctor immediately.
Distinguishing Between Healing and Deterioration
It's important to differentiate between the normal healing process and signs of a worsening ulcer. Some redness and swelling are expected initially. However, increasing redness that spreads beyond the wound edges, accompanied by a worsening odor, signals a problem.
Additionally, new or increasing pain, even if mild, should not be ignored. These changes warrant a visit to your healthcare provider.
Temperature Changes: A Subtle But Significant Warning
Temperature differences between your feet can signal a developing issue. If the foot with the ulcer feels significantly warmer than the other, it could indicate an infection.
Conversely, a foot that's colder than normal might point to poor circulation, another serious concern. Monitoring foot temperature is a simple yet important part of at-home care.
Pain Patterns: Listening to Your Body's Signals
While neuropathy can mask pain, any new or increasing pain, even if seemingly minor, needs immediate attention. This could be a throbbing, burning, or shooting pain, especially at night.
This pain could indicate a worsening infection or another serious complication. Learn more in our article about effective post-discharge wound care at home.
When to Seek Emergency Intervention
Determining when home care isn't enough requires careful observation and understanding of potential dangers. Any signs of infection, such as spreading redness, increased swelling, changes in drainage, foul odor, or fever, warrant immediate medical attention.
Don't wait to see if it gets better; prompt intervention is crucial for successful healing.
Making the Right Decision: A Practical Framework
Here’s a quick guide to help you decide when to seek professional help:
- Increasing pain: Don't dismiss any new or worsening pain, even if slight.
- Spreading redness or swelling: Inflammation extending beyond the wound is a serious sign.
- Changes in drainage: Look for changes in color, amount, or consistency. A foul smell is a major red flag.
- Fever or chills: These indicate a potential systemic infection requiring immediate medical care.
- Changes in skin temperature: A warmer or colder foot compared to the other warrants immediate attention.
Diabetic foot ulcers are a serious condition. Prompt treatment can significantly impact your healing journey. If you're uncertain, it's always best to err on the side of caution and seek professional medical advice. Rapid Wound Care offers comprehensive at-home wound care services for diabetic ulcers and other complex conditions. Our team of certified professionals utilizes advanced therapies to promote healing and improve overall well-being. Visit us today to learn more and schedule a consultation.

